Medical Treatment
Medical treatment for coronary heart disease includes drugs that alleviate symptoms by slowing the heart down, so that a limited blood supply matches less demand, or relax (dilate) arteries so that more blood can pass through, lower blood pressure so that the heart has to work less, lower cholesterol etc. etc. It also includes lifestyle modifications (diet, exercise and weight loss). No present treatment can cure CAD!
The diseases that cause CAD are determined by things such as your genes, diet, smoking and your environment.
Treatments all have the same goals: to improve quality of life and to alleviate symptoms by balancing the supply and demand of blood to the heart. Medical treatment, diet and exercise may also delay or stop the progression of the disease and thereby prolong life. However, there are some important differences between medications and life style modification on one hand and procedures on the other.
Procedures are usually more beneficial than medical treatment when there are severe blockages (stenoses) and/or when many coronary arteries are involved, or when the left main coronary artery (the artery that supplies blood to the left side of the heart) is narrowed.
Heart failure is caused by poor function of the heart (which is to pump blood to the rest of your body). If this is due to extensive damage from a previous heart attack, improving the blood supply may not help the heart function. However, if heart failure is caused by severely impaired blood supply to an otherwise viable heart muscle, restoring the blood flow back to normal may have dramatic improvement as a result. Patients with these types of heart disease benefit more from primarily bypass surgery, than from medical treatment.
Procedures
- Angioplasty, with or without stent placement, also called PTCA or PCI (Percutaneous Coronary Intervention);
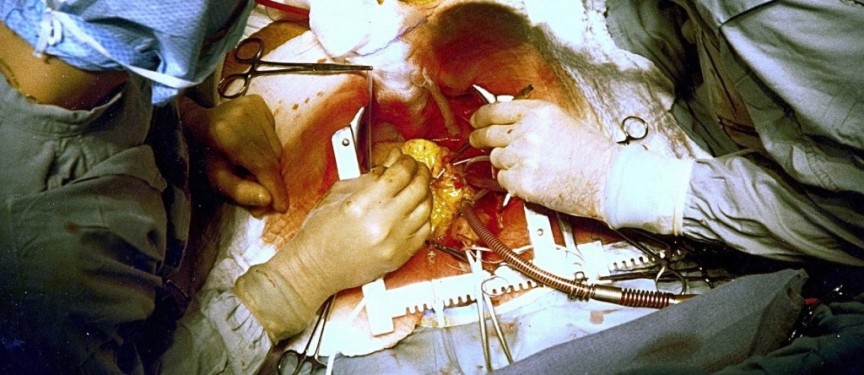
- Coronary artery bypass graft surgery (CABG).
Procedures such as PCI and CABG improve the blood supply to the heart. They do not influence the disease process that causes CAD. If successful, they effectively relieve symptoms of coronary heart disease, such as angina.
PCI uses a balloon to dilate (stretch) narrowed arteries in the heart and may include placement of a stent to hold the artery open.
CABG involves sewing one end of an artery or vein upstream to a blocked coronary artery and the other end below the blockage (stenosis), thereby allowing the blood stream to bypass the obstruction. The arteries or veins used for the bypass are like spare parts your body has for just these type of procedures. The veins are usually found in the leg and the arteries behind and parallel your breast bone (the sternum).
Indications for PCI
PCI is often recommended when arterial narrowing is moderate to severe or when only one or two coronary arteries have a stenosis. It may be less effective in patients who have diabetes, especially if there are two or three vessels involved: Persistent and intolerable symptoms despite adequate medical treatment Specific patterns of blockage and a high risk of either a heart attack or death.
Limitations of PCI
- PCI has not been shown to prolong life compared with medical therapy;
- PCI is used principally to improve angina symptoms when medications have failed;
- Although PCI restores blood flow and relieves symptoms in over 90 percent of patients, there is a risk of recurrent symptoms within six months, often due to recurrent narrowing (restenosis) of the artery.
Restenosis that is severe enough to cause bothersome or life-threatening symptoms occurs in:
- Approximately 30 percent of people who have balloon angioplasty without stent placement;
- Approximately 15 percent of people who have a bare metal stent;
- Less than 10 percent of people who have a drug coated stent.
Some coronary artery sites are more prone to re-narrowing than others. In addition, some conditions increase the risk of restenosis:
- Diabetes;
- Continued smoking;
- High blood pressure;
- Small and narrow arteries;
- High cholesterol;
- Stenosis in a major blood vessel at or near the beginning of a side branch.
Indications for CABG
Patients who have extensive coronary heart disease, including a large number of narrowed coronary arteries or narrowing of the left main coronary artery and poor pumping function of the heart tend to live longer when they have coronary artery bypass surgery rather than medical treatment.
- Patients who have at least three narrowed coronary arteries are usually advised to undergo bypass surgery;
- When the left main coronary artery (the artery that supplies blood to the left side of the heart) is narrowed;
- Patients with poor heart function;
- Patients with Diabetes and extensive CA.
Limitations of CABG
CABG restores blood flow and relieves symptoms in 95 percent of people immediately after surgery. Patients with symptomatic angina who undergo CABG can have greatly improved outcomes.
As an example, in the Coronary Artery Surgery Study (CASS) of 8221 patients undergoing CABG, 56 percent were alive at 15 years. Among those 65 and 75 years of age at the time of surgery, 15 year survival was 54 and 33 percent, which was higher than a similar age group in the United States who did not have CABG.
Reasons for recurrence of angina include graft failure and/or progression of disease in the bypassed or non-bypassed vessels. The recurrence of angina is less frequently seen when the vessel used for the bypass is an artery as compared to a vein.
By 10 years, 90 percent of arterial grafts are still open; in contrast, about one-half of all vein grafts become narrowed or occluded at 10 years after bypass surgery.
However CABG is a difficult procedure and complications may occur that will affect long term outcomes:
- Two to 4 percent of patients experience a heart attack after surgery. This occurs less frequently in patients who are low risk as compared to patients who are high risk, undergoing repeat CABG, or CABG combined with other cardiac surgery;
- Generally post-operative heart attacks are small to moderate in size;
- Low cardiac output (when a reduced volume of blood is pumped out of the heart to the body) can occur during or after surgery. This is often temporary and responds to intravenous fluids and/or a brief period of therapy to improve heart function;
- Sternal wound infection of the chest incision (called the sternal wound) occurs in approximately 1 percent of patients;
- Diabetes mellitus, obesity, and the use of both left and right internal mammary arteries increase the risk of sternal wound infection;
- Women with a history of breast cancer are at especially high risk, possibly related to therapies used during breast cancer treatment;
- Renal failure: a temporary decrease in kidney function occurs in approximately 5 to 10 percent of patients undergoing CABG.
The treatment of coronary artery disease is individualized. The information from your cardiac catheterization will help you and your doctor determine which treatment option is best for you.
Everything mentioned here is ultimately dependent on the skills of the people involved, not only of the cardiologists and cardiac surgeons involved with the procedure, but also their respective teams and the hospital. It is therefore vital that you know the answer to questions such as:
- What kind of results does your doctor have with the procedure he recommends?
- How often does a complication occur? How experienced is the team?
- What is the reputation of the hospital, doctors etc.
- Lawsuits indicate unhappy customers.
Ask for personal outcomes, not just reported data from other centers!