Two new articles, published in the July edition of Clinical Research in Cardiology, provide a point-counter point perspective by cardiac surgeons and cardiologists. In them, the proponents used the SYNTAX trial to argue their points. Not surprisingly, the authors reached opposite conclusions.
Now, how is that possible?
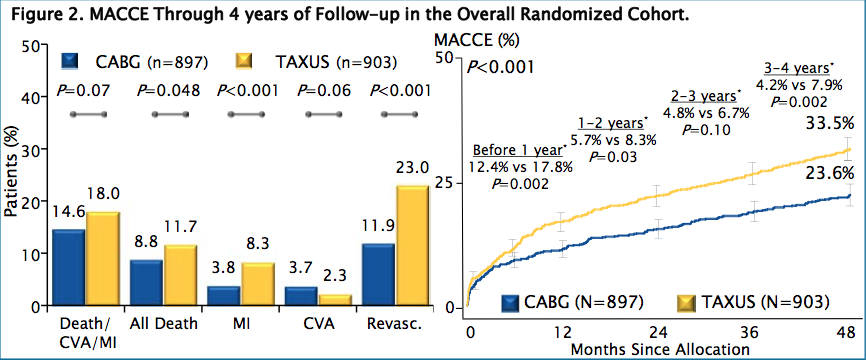
In “Patients should be operated!” Reichenspurner and colleagues argue that “…clinical trials, both observational and randomized, have proven the superiority of coronary surgery over PCI in almost every type of multivessel or left main CAD in symptomatic patients…” They end with the SYNTAX conclusion of: “… CABG remains the standard of care for patients with three-vessel or left main coronary artery Disease…’’
In “Patients should undergo PCI!” Schächinger and colleagues begin by saying:”… technical innovations have been faster than performance of clinical trials, making results of randomized studies outdated at the time of appearance…” Taking that to heart (pun intended), no study will ever report meaningful information!
However, after showing the superiority Coronary Artery Bypass (CABG) over Stenting (PCI) in two figures, they then conclude “…data favoring surgery were based on antique studies comparing CABG surgery with PTCA data from the pre-stent era…” Mind you, SYNTAX was published in 2009!
And “…With PCI, the patient is likely to come back and have another stent, but that will translate in only 1–2 additional days in hospital. With surgery, he is likely to have a good long-term solution but will have a higher risk of stroke and the inconveniencies of major surgery…” What about the repeated risks and complications of more procedures?
While a major stroke after heart surgery can be a devastating complication when it happens, in my own practice it was a very rare occurrence, certainly far below reported publications. Patients complained on occasion about their vision to the point where they might need a new prescription. While undoubtedly due to what is called a “pump head“, it was rarely the cause of major disability. “The inconvenience of major surgery” in my hospital meant that there was a “push” from the administration to discharge a routine patient three days after their operation. I strongly disagreed (way too early), but a patient with a straightforward operation and recovery was usually discharged five to seven days later. During that same period “stented” patient routinely would spend a week to ten days in the Coronary Care Unit on Heparin drips to guard again sudden complications such as thrombosis. The net result was that a Bypass patient often went home sooner than a Stented patient (and on a lot less medications)!
The authors conveniently forget not only the recurrence rate of >10% per year, but also the risks of acute withdrawal of the absolutely necessary anti-platelet drugs (with the associated extraordinary high mortality), and the fact that stenting offers no long-term survival benefit except in rare cases (“acute coronary syndromes, STEMI, and non-STEMI).
What is omitted from either article (but alluded to in “PCI”), is the fact that cardiologists controls what happens, beginning with explaining CABG as major surgery (which it is), and PCI as a minor procedure (which it isn’t), and ending with the simple fact that almost all decisions are made in the cardiac catherization laboratory to which a surgeon is rarely invited.
Early on in my career I was told by an angry cardiologist that if he wanted an opinion, he would have asked for it, after I had suggested that a patient (referred for bypass surgery) would be better off with medical therapy alone! Believe me; little has changed in the way cardiologists and cardiac surgeons interact.
There is no incentive for a cardiologist to decide for either Optimal Medical Therapy (OMT) or Coronary Artery Bypass Surgery (CABG), as I have mentioned before. Surgeons for the most part hope to be thrown a bone every now and often fight like dogs with each other to get it. In order to do so, they have fine tuned bypass surgery to the point where outcomes are better than ever, despite facing sicker and older patients.
Above all, they have to remain silent when, despite overwhelming evidence to the contrary, most patients (in non-emergent situations):
- Are talked into procedures that will not prolong their lives,
- Face repeat stenting at regular intervals,
- Face discontinuation of very expensive medications at their peril, in a society that pays for an estimated 30% unnecessary procedures.
It is no surprise that these two articles come from another country than the US, or that I have written so little about the surgical end of the spectrum of Coronary Artery Disease:
American surgeons are much too wimpy and afraid to lose even more market share than to argue with a referring cardiologist. In any case, they usually don’t even know about a potential patient and thus cannot participate in decision making.
As a result, most surgical literature is not about comparative trials, but rather about surgical technique and management. Surgeons like to prove to each other that they are better than the next guy, but in this arena too often fail to fight for what is best for their patients.
Cardiologists approach their specialty from a different point of view:
- Surgery is dangerous;
- Why send a patient to surgery if a stent can be done (repeatedly);
- A surgical opinion is only relevant when the decision for an operation has already been made;
- If all fails there is always a surgeon at their beck and call;
- Unwanted outcomes in comparative studies such as SYNTAX and COURAGE only lead to new studies attempting to disprove previous investigations;
- The economics and market share of cardiac disease dictate medical decisions.
Dr T

Comments 4
Wow…
What a strong article.
All I can say is that even in internal medicine, we ARE being trained about the negative potential effects of stenting, and most cardiology attendings I have think very carefully prior to stenting. I think things will change in 10 years.
I DO think it’s about time for surgeons to start communicating better with medicine, who indeed may have may have a bias against surgery which is unfounded.
Jane Smith, MD
Dear Dr Smith,
Glad to hear. I am not sure whether that attitude extends much beyond university hospitals with hospital based (and salaried) physicians, but remain ever hopeful you will be right some day,
Dr T
For reference, please could you suggest an approximate cost for a PCI, and the time needed for the operation? I assume it requires much less use of expensive equipment than CABG; does that make it more or less profitable for the hospital and the cardiologists, please?
Or to put the question another way, which is more profitable to the cardiologist – a PCI or a CABG?
Dear GSS,
A Stent procedure is a lot simpler to do and requires much less training than a Coronary Artery Bypass (CABG) operation. Each stent (especially the new drug eluting stents) costs to my knowledge approximately $2000. Often multiple stents are needed, in addition to which a patient faces $2-3000/year of medications (and thus income to yet another pharmaceutical industry).
Stenting is much more profitable to hospitals than CABG, especially if the >10%/year need for a repeat procedure is taken into account.
If a patient is submitted for CABG, the surgeon gets reimbursed for the procedure rather than the cardiologist. That is why there is a lot of incentive to do as many stents as possible and only refer a patient for surgery when this is no longer feasible.
Remember that most patients don’t need another operation after CABG and are thus lost as a source of income!
Dr T