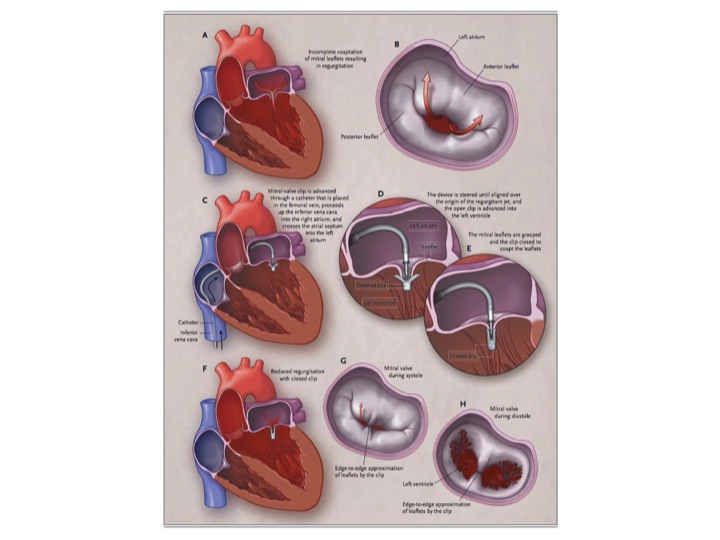
Percutaneous Repair or Surgery for Mitral Regurgitation (the EVEREST II study), published in the NEJM on April 4th, compares the use of a mitral-valve clip with traditional surgery for repair or replacement of a leaking mitral valve.
The authors concluded: “Although percutaneous repair was less effective at reducing mitral regurgitation than conventional surgery, the procedure was associated with superior safety and similar improvements in clinical outcomes.”
This is a surprising solution, given the fact that the procedure was associated with:
- 6% operative mortality (plus an additional 1% at 30 days)
- 20% need for conversion to a conventional procedure
- 27% 2+ mitral regurgitation
- 21% Grade 3+ or 4+ mitral regurgitation
The surgical results were hardly impressive either:
- 6% operative mortality (plus an additional 2% 30-day mortality!)
- 20% Grade 3+ or 4+ mitral regurgitation
Subgroup Analysis for the Primary End Point at 12 Months showed superior performance of surgery vs. percutaneous repair (freedom from death, from mitral-valve surgery, and from grade 3+ or 4+ mitral regurgitation), with all subgroups doing better with surgery.
The authors conclude (again):
“Although percutaneous repair was less effective at reducing mitral regurgitation than surgery before hospital discharge, at 12 and 24 months the rates of reduction in mitral regurgitation were similar, and percutaneous treatment was associated with increased safety, improved left ventricular dimensions, and clinical improvements in NYHA class and quality of life.”
In striking contrast, a 99% success rate and an operative mortality of 1 % for mitral valve repair has been documented in a number of publications from major institutions around the world.
This was a prospective, randomized study, and thus acutely ill patients were excluded, as well as those with poor LV function, which might otherwise have explained a high peri-procedural mortality. What is not explained however, is the high mortality, both in the percutaneous and surgical groups. These were not patients, too ill to undergo a conventional repair, and therefore it was even more surprising the surgery arm of the study included mirtal valve replacement at all!
Likewise, because of limitations associated with the device, anatomic requirements included a centrally located mal-coaptation of the mitral leaflets causing the regurgitation. Mitral regurgitation is caused by a host of different anatomic abnormalities and thus requires a variety of repairs, very unlike this cookie-cutter approach. This alone might explain some of the poor functional results.
It is thus hard to believe the authors dared to defend, let alone compare their results with outcomes published elsewhere (carefully omitted from the bibliography). The Society of Thoracic Surgeons (STS) has set a benchmark for mitral valve repair of 1.1% as a standard for any surgeon performing this type of procedure. Any new repair technique needs to be measured against this.
An editorial in the same NEJM issue stated: “As compared with mitral-valve surgery, the mitral clip was associated with a lower rate of complications at 30 days. However, it is disappointing that by 1 year after the procedure, 20% of patients in the percutaneous-treatment group required surgery for mitral-valve dysfunction, as compared with 2% of patients in the surgical group who required repeat surgery.”
Is it possible the authors were unaware of the excellent results that have been published with mitral valve repair? Not discuss a mortality 700% greater than the well known standard procedure; recurrence rates of 20%? I find this hard to believe!
Please tell me what you think,
Dr T
http://www.cardiac-risk-assessment.com/