Anatomy | Pericardial effusion | Pericarditis | Causes | Treatment
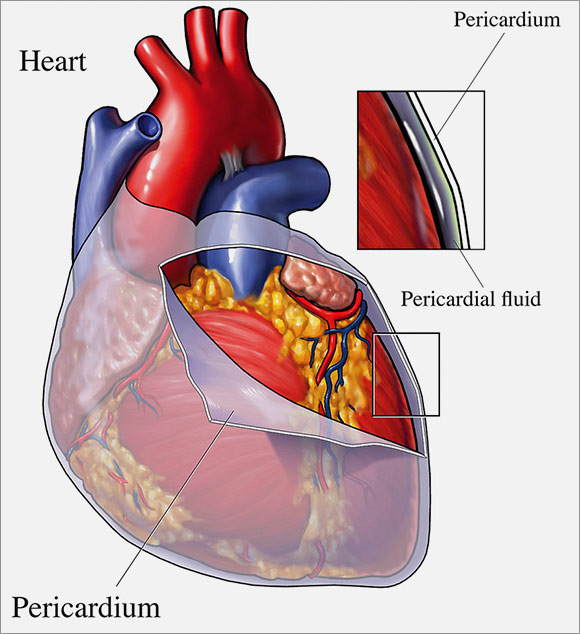
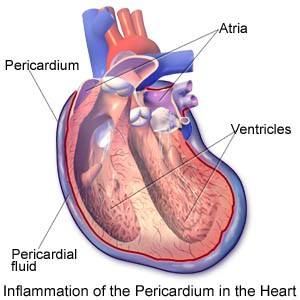
Your pericardium is a thin double-layered sac which encloses the heart, and the large blood vessels that enter and leave the heart. The pericardium keeps the heart contained and protected within the chest cavity. Fluid within the pericardium surrounds the heart and lubricates its surface. This makes it possible for the heart to move (beat) within this small space.
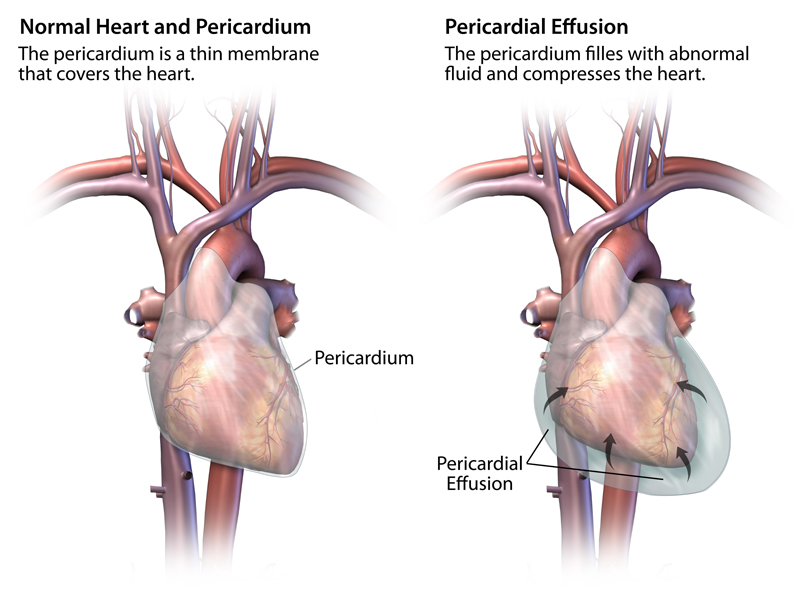
When more than a little fluid accumulates around the heart it is called a pericardial effusion. If it happens over a long period of time the pericardium can stretch, but if it happens abruptly, such as after an injury, there is not enough room for more fluid and the heart at the same time. Under such circumstances the heart gets compressed, which prevents blood from returning into the heart. Less in, means less out and the result is poor heart function and a drop in blood pressure. If left untreated, pericardial effusion can cause heart failure or death. This condition is called Cardiac Tamponade. Tamponade is a life-threatening condition if left untreated.
Pericardial effusion symptoms may include:
- Shortness of breath or difficulty breathing (dyspnea)
- Shortness of breath when lying down (orthopnea)
- Chest pain, usually behind the breastbone or on the left side of the chest
- Cough
- Painful breathing, especially when inhaling or lying down
- Fainting or dizziness
- Low-grade fever
- Rapid heart rate
- Overall sense of fatigue or weakness
You can have significant pericardial effusion and experience no signs or symptoms, particularly if the fluid has increased slowly. This is more common when the cause of pericardial effusion is cancer or a chronic inflammatory disorder, such as rheumatoid arthritis.
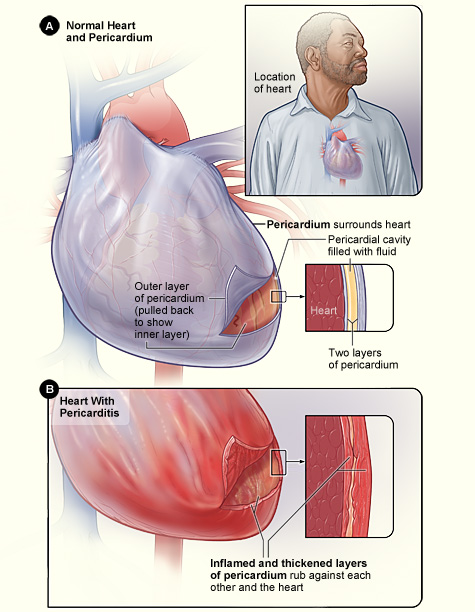
Pericarditis is inflammation of the pericardium. The pericardium has an inner and outer layer with a small amount of lubricating fluid between them. When the pericardium becomes inflamed, the amount of fluid between the two layers increases. This squeezes the heart and restricts its action.
Pericarditis can result from one or more of these:
- a viral, bacterial or fungal infection
- heart attack
- cancer spreading from a nearby tumor in the lung, breast or the blood
- radiation treatment
- injury or surgery
Sometimes it accompanies other diseases like rheumatoid arthritis, lupus and kidney failure.
Symptoms of pericarditis
Chest pain is common, especially pain behind the breastbone. Sometimes this pain spreads to the neck and left shoulder. Pain from pericarditis often is a sharp, piercing pain over the center or left side of the chest. The pain may get worse with a deep breath. Less often the pain is dull. A fever is also common. Patients with pericarditis feel sick as opposed to angina type pains.
Analgesics or anti-inflammatory drugs are given to relieve pain. Antibiotics are also prescribed if the pericarditis is due to a bacterial infection. If excess fluid is seriously affecting the heart’s action, a needle may be used to draw it off. In some cases surgery may be required.
Acute inflammatory pericarditis usually lasts one to three weeks and doesn’t lead to further problems. About 20% of pericarditis patients have a recurrence within months or, rarely, within years.
Sometimes a chronic form of pericarditis can develop into intense scarring (“constrictive pericarditis”) that prevents the heart from pumping, a condition in which a diseased and stiffened pericardium is impairing normal cardiac function, not unlike from what happens with cardiac tamponade.
Since blood has trouble returning to the heart (impaired filling), the heart function becomes progressively limited with symptoms of heart failure that include
- Edema,
- Shortness of breath
- Pain
When that occurs, the only treatment is a “pericardiectomy”, the surgical removal of part or most of the pericardium from the surface of the heart, a difficult and sometimes dangerous operation. If the underlying heart function is adequate, significant improvements are possible.

Comments 3
I am 4 months post-op. I had a CABG x 2. I find this fascinating. The pericardium was cut to allow the surgeon to perform the bypass graph. I don’t think that the pericardium is sewen up.
1. Are there complications If it is left open.
2. Will the pericardium grow back by itself?
Thank you, PHB
What a great question. I have been searching for the same answer.
My pericardium was removed due to an effusion of 1,250ml of fluid and jelly, 3 weeks after an Aortic valve replacement. I was very lucky!
Now with COVID-19 in the population, I am concerned that my heart is more vulnerable to this virus as there may be no pericardium and I should be extra vigilant.
Pingback: Pericarditis and pericardial effusion - Cardiac Health