Carcinoma of the esophagus is a relatively rare but very lethal disease. 50% of all patients diagnosed will have adeno carcinoma, which has been associated with a very poor long term survival.
During my residency, I had the honor of working with F. Henry Ellis, one of the giants of esophageal surgery in the US. Yet even he confessed that a successful operation would only prolong life by about six months, as the patient would invariably die of recurrences elsewhere. At a time when the operation was associated with a high morbidity and mortality, he stressed the importance of a smooth and uneventful recovery, as any survival benefit would be eliminated by a major complication. I remember a national meeting where, as a panel member, he was asked how he dealt with complications. He answered bluntly to redirect this question to another panelist, as he had too little experience with complications to be able to answer this question.
As a result, I was used to operating a patient, feeding him on day 3, and send him home on day 7 after surgery. Although rare, complications occurred occasionally, just like they did on Dr. Ellis’s service, much as he would like to deny this!
While agreeing totally on surgical technique, I could not help thinking there had to be the possibility of better outcomes than a short term prolongation of life. This then led to treatment which included post operative chemo-radiation therapy. I had a hard time convincing the local oncologists of this approach (radiation oncologists needed not to be convinced), but ultimately prevailed. A compromise that drove me crazy was the constant change in agents that made an evaluation of success so much more complicated.
This then is the long term follow-up of all patients treated in my practice from 1983-2001 for Carcinoma of the Esophagus. One of the many advantages of living in Maine included an ability of follow-up that simply is not possible in many other parts of the country. As a result I was able to continue to collect information about my patients throughout my career.
Background
A review of the literature showed the following:
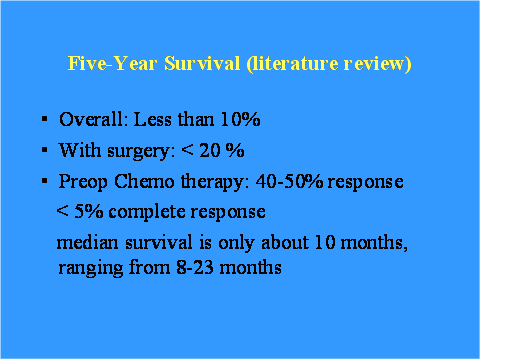
In 2001, I reviewed a number of series:
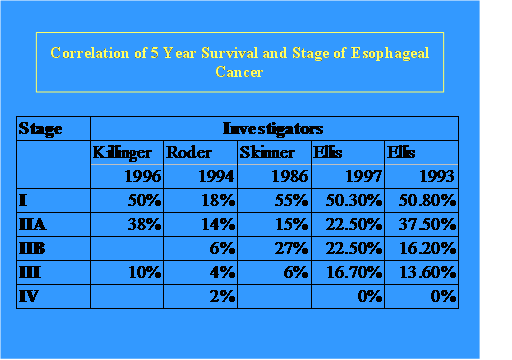
I participated in both of Ellis’s publications as a resident at the New England Deaconess Hospital in Boston, Mass, and used this as the basis for analysis of my own patients.
MUCH to my surprise, not much has changed in 2010:
| Median survival duration and 3-year survival rate with and | ||||||
| without neoadjuvant therapy for esophageal carcinoma | ||||||
| Median survival | 3-year survival | |||||
| (Months) | (Months) rate (%) | |||||
| Trial | N | Surgery | Neo + surg | Surgery | Neo + surg | P value |
| Walsh (1996) | 113 | 11 | 16 | 26 | 37 | <0.01 |
| Law (1997) | 147 | 13 | 16.8 | 31 | 44 | NS |
| Kelsen (1998) | 467 | 16.1 | 14.9 | 37 | 35 | NS |
| Clark (2001) | 802 | 13.3 | 17.2 | 34 | 43 | NS |
| Ancona (2001) | 96 | 24 | 25 | 41 | 44 | NS |
| Neo indicates neoadjuvant chemotherapy plus radiation; surg, surgery; NS, not significant. | ||||||
Results & Analysis
From 1983-2000, 158 consecutive patients underwent surgery for carcinoma of the esophagus, 94% of whom had an adeno carcinoma. Characteristic are listed below:
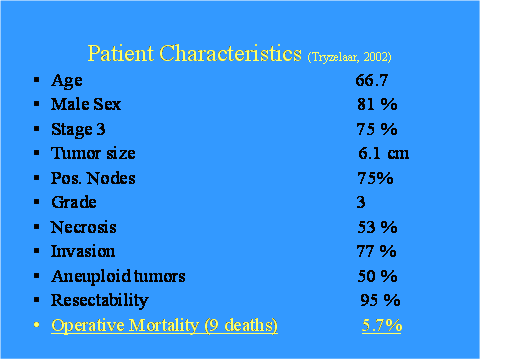
Most patients were male and had advanced disease at the time of surgery and were successfully operated (95%).
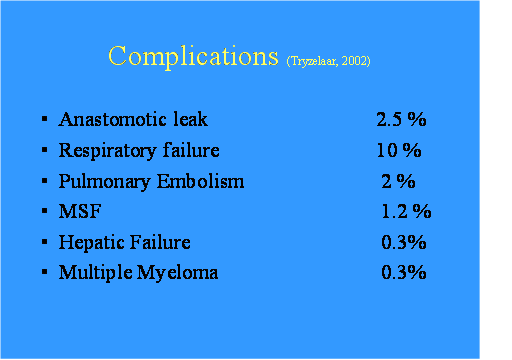
To my sorrow, complications did occur despite my mentor’s remonstrations. One explanation may well be the advanced nature of disease and the technical problems this presented in some of the patients. There were 4 leaks, a disastrous complication if and when it happens and one case of acute hepatic failure, the cause of which still baffles me. Invariably, a complication was very time consuming to treat and interrupted the speedy transition to adjuvant therapy needed for long term control. As a result I continue to echo Dr. Ellis’s caveat of avoiding complications!
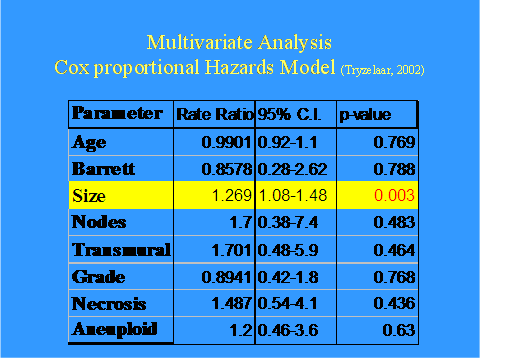
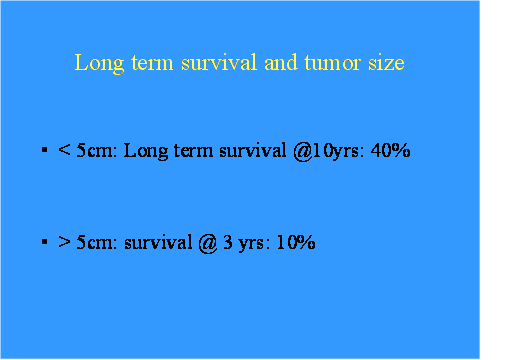
Analysis of the outcomes did yield one predictor of poor long term survival: Primary Tumor size > 5cm:
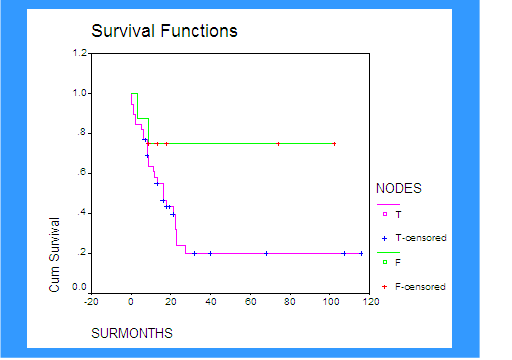
Kaplan Meier Survival analysis
Tumor size, the one risk factor that became a predictor of poor survival:
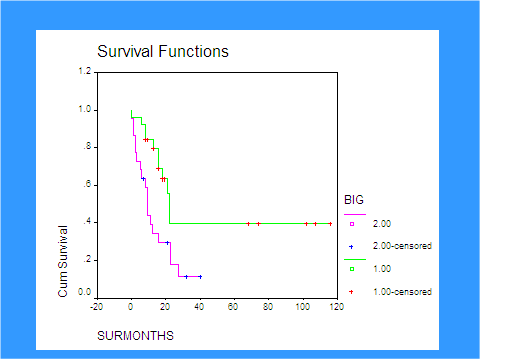
The green curve stands for tumors smaller than 5cm in length, however, some long term survival benefit was present even in patients with large tumors.
Survival by stage:
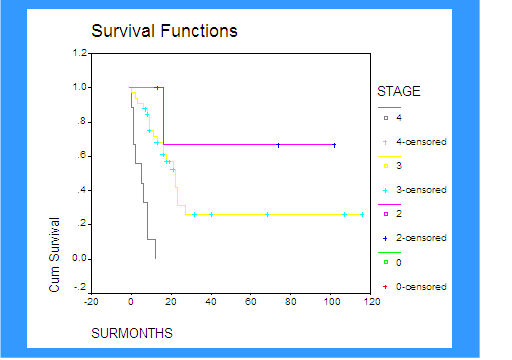
There was a big survival difference between stage I and II tumors with III and IV. Stage II meant IIB small tumors with positive lnn!
A comparison with Cleveland Clinic (2003) shows a favorable outcome difference:
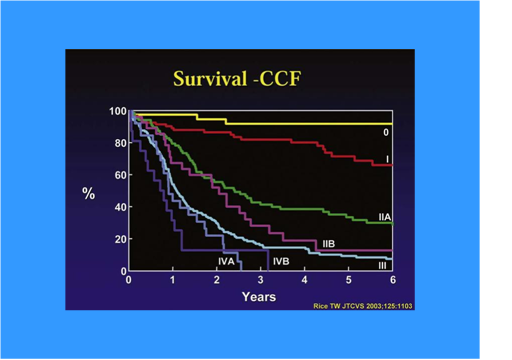
In my series patients with IIB disease had an >60% survival at 10 years, vs. <20% at five years in CC data.Likewise, stage III patients survived had about 26% survival rates vs. what appears <10%.
Nodal status showed an obvious survival difference but statistically insignificant, presumably because almost all patients had positive nodes at the time of resection:
Conclusions
Long term survival is possible in patients with advanced adenocarcinoma of the esophagus:
- TNM staging accurately predicts outcome
- Survival is strongly related to tumor size
- Long term survival after resection is probably the result of adjuvant therapy
- DNA analysis was not predictive of long term survival
In this series tumor size (and the absence of peri-operative complications) was the one strong predictor of long term survival:
And:
- Aggressive Surgical Therapy is strongly indicated in the treatment of Adenocarcinoma of the Esophagus
- Low perioperative mortality and morbidity rates are necessary to allow speedy initiation of adjunct therapy
- Long term survival depends on early discovery, and the combination of all treatment modalities available
This study compares favorably with other reports in the literature:
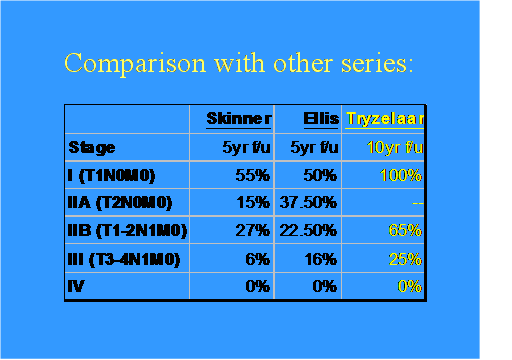
Differences in survival rates are most likely explained the presence or absence of adjuvant therapy.
Dr T

Comments 2
Joanne was diagnosed on March 28 2017 with Adenocarcinoma of the Esophagus finding a lower esophagus tumor and the source of pain was Adenocarcinoma in the mucus-secreting glands in the lower esophagus. She had radiation on the tumor but no surgery. She started FolFox4 chemo each 2 weeks than moved out after three years to 3 weeks. The cancer had spread to her right knee and she had the joint replaced and some additional radiation treatment. After about a year cancer spread to her brain and she had whole brain radiation treatments. She died 5 May 2021 when the cancer had gotten into her spine causing some memory issues, muscle weakness and pain in her back and hips. This new cancer was not found until a MRI was preformed about two weeks before she died in hospice.
Pingback: The MASS II Study - Cardiac Health