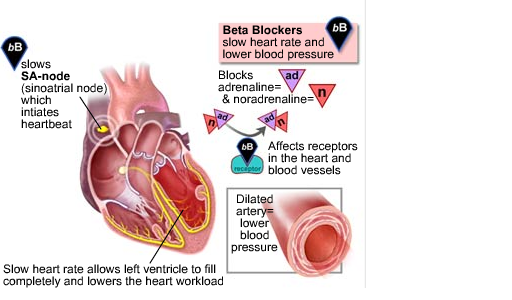
Beta (β) blockers stop the action of epinephrine (adrenaline) and norepinephrine (noradrenaline) on so-called β-adrenergic receptors, part of the sympathetic nervous system which mediates the “fight or flight” response. If you feel this “skipped beat” every time you take your Propranolol, it is most likely an indication it has “kicked in” and started doing its job.
Beta blockers inhibit these normal epinephrine-mediated sympathetic actions. They reduce the effect of excitement/physical exertion on heart rate and force of contraction, dilation of blood vessels, opening of bronchi, reduce tremor, and breakdown of glycogen.
The antihypertensive mechanism appears to involve: reduction in cardiac work and a central nervous system effect to reduce sympathetic activity.
Antianginal effects result from making the heart work less and thereby reduce its demand for oxygen.
The antiarrhythmic effects of beta blockers arise from sympathetic nervous system blockade:
Indications for beta blockers include:
- Hypertension
- Angina
- Cardiac arrhythmia
- Congestive heart failure
- Myocardial infarction
- Glaucoma
- Migraine prophylaxis
- Symptomatic control (tachycardia, tremor) in anxiety and hyperthyroidism
- Essential tremor
- Phaeochromocytoma, in conjunction with α-blocker
Beta blockers perform less well than other drugs, particularly in the elderly, and there is increasing evidence that the most frequently used beta-blockers at usual doses carry a risk of provoking type 2 diabetes.
Side effects
Common adverse drug reactions of beta blockers include: nausea, diarrhoea, bronchospasm, dyspnoea, cold extremities, exacerbation of Raynaud’s syndrome, bradycardia, hypotension, heart failure, heart block, fatigue, dizziness, abnormal vision, decreased concentration, hallucinations, insomnia, nightmares, depression, sexual dysfunction, erectile dysfunction and/or alteration of glucose and lipid metabolism.
About 10% of patients treated with beta-blockers may become dizzy or light-headed. More seriously, about 5% may become clinically depressed, with feelings of helplessness and hopelessness that sometimes lead to suicide. As might be expected, all such reactions are less common with beta-blockers that do not enter the brain readily.
Other moderately common side effects of beta-blockers include diarrhea, rash, slow heartbeat, and impotence or loss of sexual drive.
An additional concern with beta-blockers is their effect on blood cholesterol, they lower the amount of “good” (HDL) cholesterol, while increasing the amount of “bad” (LDL) cholesterol. They also raise the amounts of fatty materials known as triglycerides in the bloodstream; some scientists believe triglycerides may increase the risk of a heart attack to almost the same extent as cholesterol. Nevertheless, there is no concrete evidence that people treated with beta-blockers are more likely to have heart attacks than those treated with other blood-pressure medications.