Ventricular Septal Defect (VSD)
A Ventricular Septal Defect (VSD) is the second most common cardiac malformation, accounting for approximately one fifth of all congenital cardiac anomalies. VSD also occurs in combination with other congenital heart defects, as in an atrioventricular canal (AVC), tetralogy of Fallot (TOF) and occasionally, transposition of the great arteries (TGA).
Anatomy
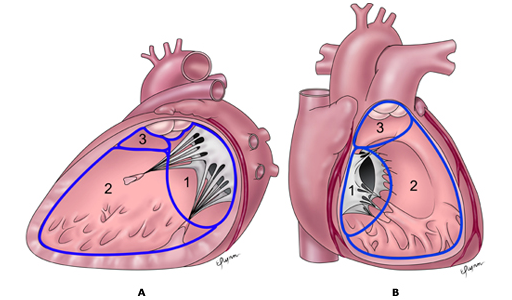
A schematic presentation of the three main anatomic components of the interventricular septum as seen from the morphologic left ventricle (A) and the morphologic right ventricle (B).
- septum of the atrioventricular canal;
- septum of the muscular septum; and
- parietal band or distal conal septum.
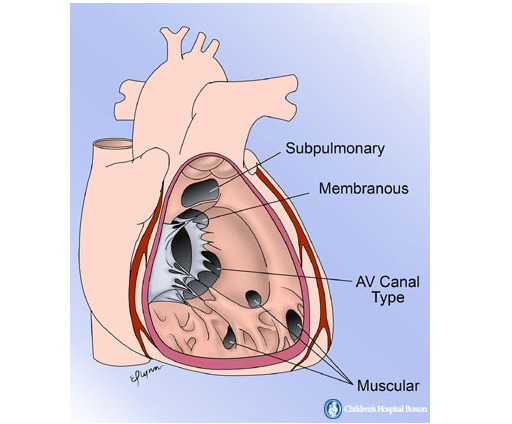
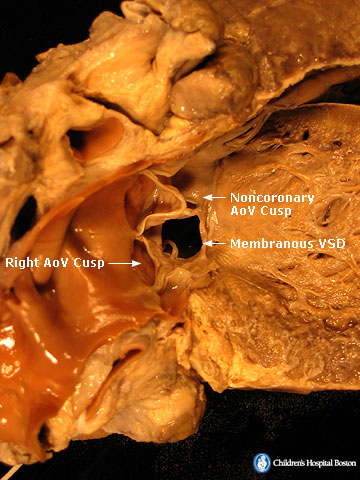
Anatomic drawing showing the location of the different types of ventricular septal defects. Sub-pulmonary defects are caused by deficiency of the conal septum. Membranous defects are located behind the septal leaflet of the tricuspid valve. Atrio-ventricular (AV) canal type defects are caused by deficiency of the endocardial cushion component of the inter-ventricular septum. Muscular defects can occur in any portion of the muscular septum. Membranous VSDs are the most common type (about 80%). Membranous VSDs lie just beneath the aortic valve and behind the septal leaflet of the tricuspid valve.
Membranous VSD, LV view:
Membranous VSD, RV view: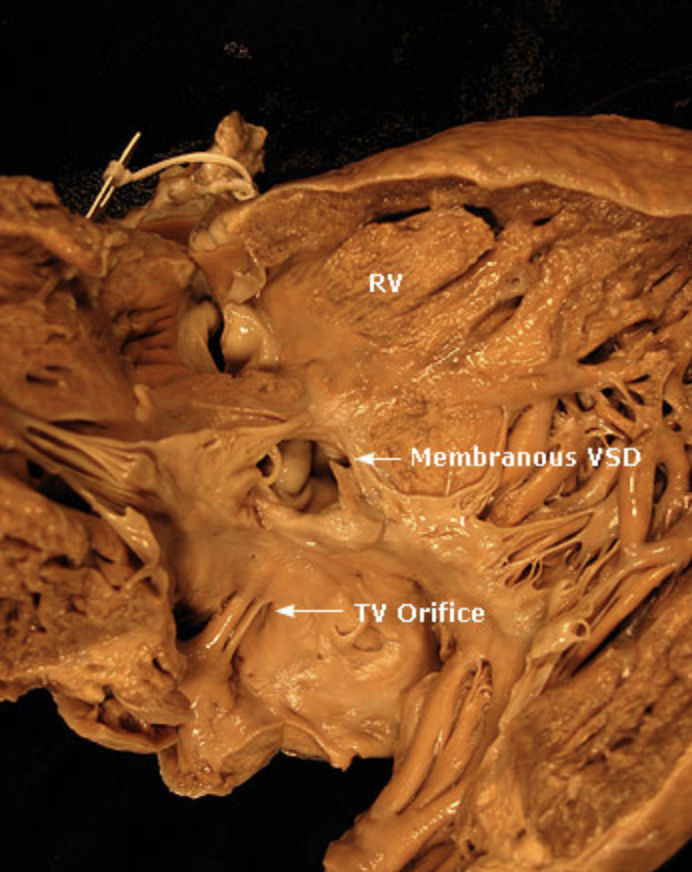
Pathophysiology and Presentation
Small VSDs (also called restrictive VSDs) frequently close spontaneously. Children with larger VSDs and greater left-to-right shunting present with the signs and symptoms of CHF. If pulmonary blood flow magnitude is high, pulmonary edema develops.
VSDs produce a characteristic systolic murmur and are often associated with recurrent upper respiratory infections poor nutrition and failure to thrive.
Most infants with VSD present in the neonatal period. The typical presentation of a small VSD in a neonate involves the detection of a cardiac murmur at four to ten days of life. Other symptoms are usually absent. Mild tachycardia and tachypnea may develop by two to eight weeks of age if the defect is larger than small, particularly with an intercurrent respiratory infection
A hemodynamically significant VSD causes excess pulmonary blood flow. The size of the VSD and the level of pulmonary vascular resistance (PVR) determine the degree of pulmonary over-circulation. Flow from the left ventricle (systemic circulation) to the right ventricle (pulmonary circulation) creates a left-to-right shunt at the ventricular level. Additionally, a large VSD causes pulmonary hypertension. Early consequences of pulmonary over-circulation create a picture of congestive heart failure (CHF).
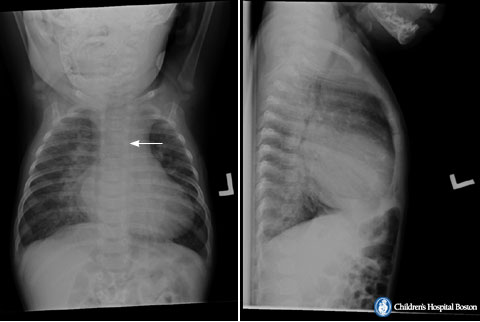
A 4-month-old infant with large membranous ventricular septal defect and failure to thrive. An anterior-posterior chest radiograph (left panel) shows situs solitus, moderate cardiomegaly, symmetrically increased pulmonary blood flow, hyperinflation, and a left aortic arch (arrow points to slight indentation of left side of trachea by the aortic arch).
Diagnosis
The diagnosis of isolated VSD is usually suspected clinically and may be confirmed with echocardiography.
Treatment
Infants with heart failure should undergo non-invasive anatomic evaluation. If failure does not respond to medical therapy, complete repair is indicated.
Trans-catheter closure of VSDs is difficult. At the present time, the complications rate for trans-catheter closure for membranous defects is greater than that of surgical closure: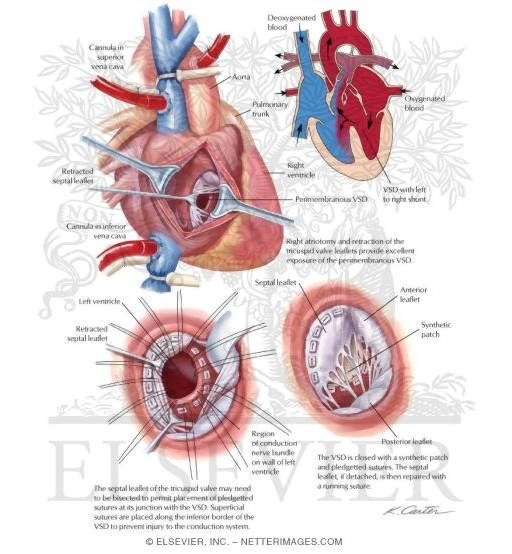
PDA
PDA accounts for 5 to 10% of congenital heart anomalies; the male: female ratio is 1:3. PDA is very common among premature infants (in 45% with birth weight < 1750 g; in about 80% with birth weight < 1200 g). A significant PDA causes heart failure (HF) in 15% of premature infants with birth weight < 1750 g and in 40 to 50% of infants with birth weight < 1500 g.
Atrial Septal Defect
The Foramen Ovale in Fetal Circulation
Before birth, the fetal circulatory system includes three open structures through which blood moves that normally close soon after birth. These structures are the ductus arteriosus, the ductus venosus, and the foramen ovale. The foramen ovale allows the shunting of blood from the right atrium into the left atrium.
VSD
A Ventricular Septal Defect (VSD) is the second most common cardiac malformation, accounting for approximately one fifth of all congenital cardiac anomalies. VSD also occurs in combination with other congenital heart defects, as in an atrioventricular canal (AVC), tetralogy of Fallot (TOF) and occasionally, transposition of the great arteries (TGA).


Comments 2
Pingback: Atrial Septal Defect - Cardiac Health
Pingback: Cardiac Defects with a Left to Right Shunt (Acyanotic) - Cardiac Health