The BARI 2D Study Group. A randomized trial of therapies for type 2 diabetes and coronary artery disease
In this study, the authors report the findings of the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial, involving 2368 patients with both diabetes and coronary disease.
Patients with type 2 diabetes and stable ischemic heart disease were randomly assigned to early revascularization plus intensive medical therapy or intensive medical therapy alone. For patients randomized to revascularization, the treating physician decided whether PCI or CABG was more appropriate. The drug treatments were also randomly assigned to either insulin-provision therapy or insulin-sensitization therapy.
Results
At 5 years, rates of survival did not differ significantly between the revascularization group (88.3%) and the medical-therapy group (87.8%, P=0.97) or between the insulin-sensitization group (88.2%) and the insulin-provision group (87.9%, P=0.89). The rates of freedom from major cardiovascular events also did not differ significantly among the groups: 77.2% in the revascularization group and 75.9% in the medical-treatment group (P=0.70) and 77.7% in the insulin-sensitization group and 75.4% in the insulin-provision group (P=0.13). In the PCI stratum, there was no significant difference in primary end points between the revascularization group and the medical-therapy group. In the CABG stratum, the rate of major cardiovascular events was significantly lower in the revascularization group (22.4%) than in the medical-therapy group (30.5%, P=0.01; P=0.002 for interaction between stratum and study group). Adverse events and serious adverse events were generally similar among the groups, although severe hypoglycemia was more frequent in the insulin-provision group (9.2%) than in the insulin-sensitization group (5.9%, P=0.003).
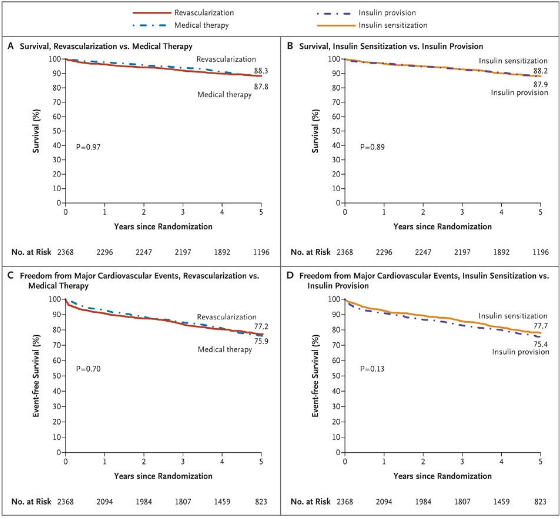
There was no significant difference in rates of survival between the revascularization group and the medical-therapy group (Panel A) and between the insulin-sensitization group and the insulin-provision group (Panel B). The rates of major cardiovascular events (death, myocardial infarction, or stroke) also did not differ significantly between the revascularization group and the medical-therapy group (Panel C) or between the insulin-sensitization group and the insulin-provision group (Panel D).
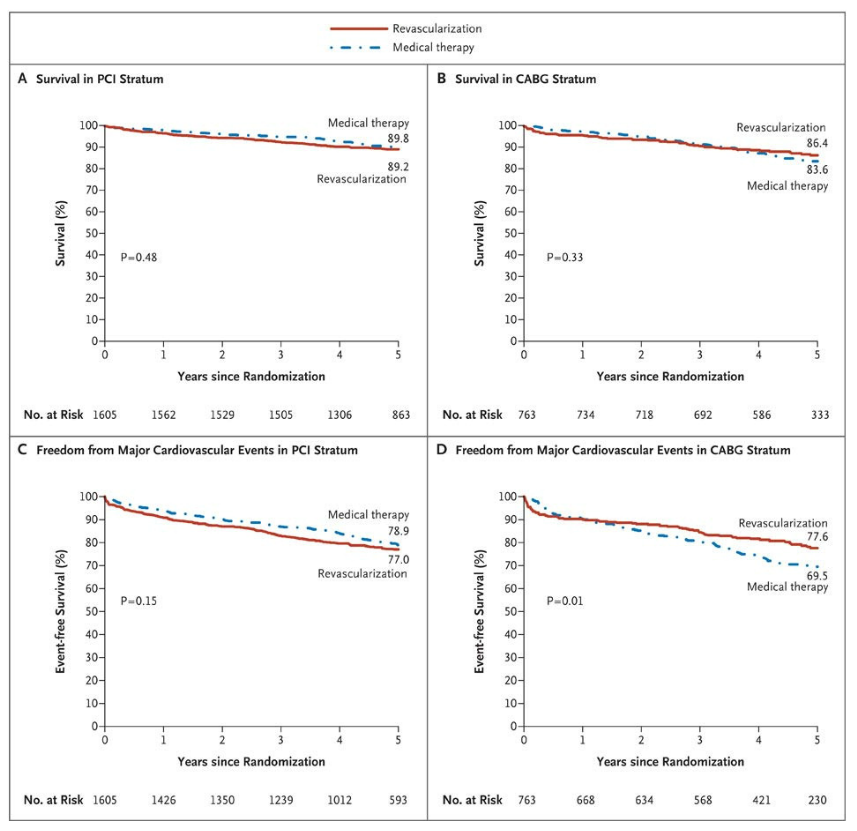
There was no significant difference in rates of survival between the revascularization group and the medical-therapy group among patients who were selected for the percutaneous coronary intervention (PCI) stratum (Panel A) or among those who were selected for the coronary-artery bypass grafting (CABG) stratum (Panel B). The rates of freedom from major cardiovascular events (death, myocardial infarction, or stroke) also did not differ significantly between the revascularization group and the medical-therapy group among patients in the PCI stratum (Panel C), but the rates were significantly better among patients in the revascularization group than in the medical-therapy group within the CABG stratum (Panel D)
Comments
BARI 2D underscores how major advances in PCI, CABG, and optimal medical therapy have created a constantly moving target against which the comparative effectiveness of rapidly evolving treatments must be repeatedly assessed. Will the results of BARI 2D change clinical practice? In the United States, the use of PCI, particularly with drug-eluting stents, remains high (1.2 million procedures per year). Yet, as health
care costs continue to spiral upward, physicians, payers, and health economists need to make informed, evidence-based treatment decisions that improve both symptoms and clinical outcomes. BARI 2D shows that for many patients with both diabetes and coronary disease, optimal medical therapy rather than any intervention is an excellent first-line strategy, particularly for those with less severe disease. When revascularization is indicated, both BARI 2D and other studies support the use of CABG as the preferred approach, unless or until future studies indicate otherwise.
Finally, although the results of any randomized trial must be individualized for specific patients, a “multidisciplinary team approach” to clinical decision making, as originally advocated by Simoons and used successfully in a recent trial, can ensure that all therapeutic options (optimal medical therapy, PCI, and CABG) are fully and transparently discussed so that patients are offered the most appropriate, evidence-based treatment recommendations.
References:
1: A Randomized Trial of Therapies for Type 2 Diabetes and Coronary Artery Disease, The BARI 2D Study Group. N Engl J Med 2009; 360:2503-2515
2. Diabetes with Coronary Disease — A Moving Target amid Evolving Therapies? William E. Boden, M.D., and David P. Taggart, M.D., Ph.D., N Engl J Med 2009 360;24,2570-2572

Comments 3
Pingback: Physical Activity and Weight Gain Prevention - Cardiac Health
Pingback: The MASS II Study - Cardiac Health
Pingback: Optimal Medical Therapy with or without PCI for Stable Coronary Disease - Cardiac Health