Calculate Your Risk for Heart Disease and Stroke with Hypertension
Hypertension is one of the most important risk factors for Coronary Artery Disease (CAD). Hypertensive patients have double the risk of CAD compared with patients with a normal blood pressure.
If you have high blood pressure (hypertension), it is important to attempt to identify and exclude reversible (secondary) causes.
|
High blood pressure guidelines |
|
|
Classification |
Blood pressure |
|
High |
140/90 or above |
|
Prehypertension |
120/80 to 139/89 |
|
Normal |
119/79 or below |
Investigations commonly performed in newly diagnosed hypertension:
- Over 91% of adult hypertension has no clear cause and is therefore called essential/primary hypertension. Often, it is part of the metabolic “syndrome X” in patients with insulin resistance: it occurs in combination with diabetes mellitus (type 2), combined hyperlipidemia and central obesity.
- Secondary hypertension is more common in preadolescent children, with most cases caused by renal disease. Primary or essential hypertension is more common in adolescents and has multiple risk factors, including obesity and a family history of hypertension.
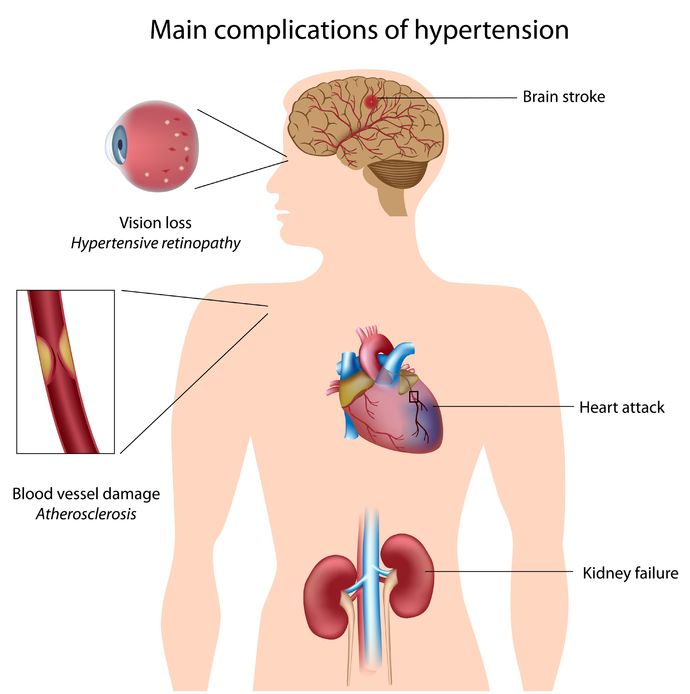
Tests are undertaken to identify possible causes of secondary hypertension, and seek evidence for end-organ damage to the heart itself or the eyes (retina) and kidneys. Diabetes and raised cholesterol levels being additional risk factors for the development of cardiovascular disease are also tested for as they will also require management.
Tests commonly performed include:
- Creatinine
- Electrolytes
- Glucose
- Cholesterol
- UA
- EKG
- Chest X-ray
(From: National Heart, Lung, and Blood Institute, hypertension guidelines)
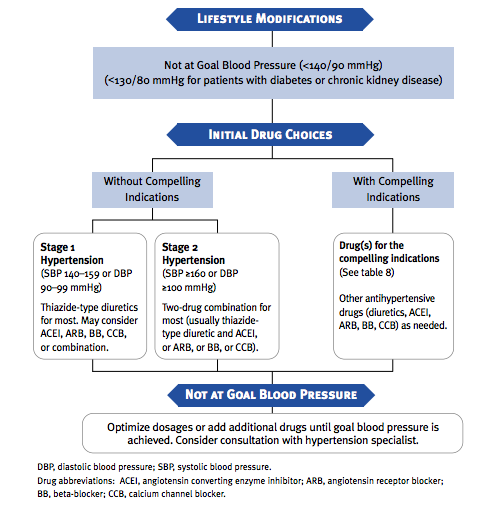
The major goal of high blood pressure (antihypertensive) therapy is the reduction of cardiovascular disease (including stroke). In most persons with hypertension, especially those age >50 years, the primary focus should be on achieving a blood pressure <140/90 mmHg since that is directly associated with a decrease in CVD complications. In patients with hypertension and diabetes or renal disease, the BP goal is <130/80 mmHg.
Initial treatment
If you fall into the prehypertension range (120–139/80–89), your doctor will likely recommend lifestyle changes, including:
- Lose excess weight
- Exercise
- Limit alcohol to 2 drinks a day for men and 1 drink a day for women.
- Cut back on salt.
- Quit smoking.
- Follow the Dietary Approaches to Stop Hypertension (DASH) diet.
The DASH eating plan is a low-fat and low-saturated-fat diet that emphasizes eating more fruits, vegetables, whole grains, and low-fat dairy foods.
Adoption of healthy lifestyles by all persons is critical for the prevention of high BP and is an indispensable part of the management of those with hypertension. Major lifestyle modifications shown to lower BP include weight reduction in those individuals who are overweight or obese, and includes adoption of a diet rich in potassium and calcium, dietary sodium reduction, increased physical activity and moderation of alcohol consumption.
There is evidence that reduction of the blood pressure by 5-6 mmHg can decrease the risk of stroke by 40%, of coronary heart disease by 15-20%, and reduces the likelihood of dementia, heart failure, and mortality from vascular disease.
Treatment for Hypertension with medications
Blood pressure drugs are prescribed to help lower blood pressure when appropriate diet and regular physical activity alone have not succeeded. They do this by helping relax and relax (dilate) blood vessels, allowing blood to flow more easily, or by acting on the kidneys to help increase urination. Some of the more common blood pressure drugs include diuretics, angiotensin-converting enzyme (ACE) inhibitors, angiotensin-2 receptor blockers (ARB), beta-blockers (BB) and calcium channel blockers (CCB). Some of these may also be prescribed for heart failure and arrhythmia patients.
THE PROPER HIGH BLOOD PRESSURE MEDICATION FOR YOU
A healthcare provider will take several factors into account when determining which antihypertensive drug should be tried first. In addition to considering the effectiveness and potential side effects, he or she will consider the person’s general health, sex, age, and race; the severity of the high blood pressure; any additional, underlying medical conditions; and whether particular drugs should not be used.
Certain antihypertensive drugs are specifically recommended for the treatment of particular conditions, even if the person does not have high blood pressure. In many cases, a person with one of these conditions also has high blood pressure. As examples:
- An ACE inhibitor is recommended for people with diabetes mellitus who have increased levels of protein in the urine (proteinuria), heart failure, or a prior heart attack.
- Beta blockers are recommended for people with heart failure or a prior heart attack.
- Beta blockers or calcium channel blockers are recommended to control symptoms in people with angina pectoris, which is temporary chest pain caused by an inadequate oxygen supply to heart muscle in patients with coronary artery disease.
There are also certain antihypertensive agents that are not recommended in some people. Some examples include:
- ACE inhibitors and ARBs (and many other medications not used to treat high blood pressure) are not recommended during pregnancy.
- Beta blockers may not be recommended for people with asthma or chronic lung disease and as primary therapy for high blood pressure, particularly in patients over age 60.
Finally, certain underlying medical conditions may be worsened by treatment with particular high blood pressure medications. As an example, diuretics can worsen gout.
Thus, it is important to mention all current and previous medical problems to the healthcare provider to determine which medication is best.
The Best Drug is the One that Works!
The “best” drug for you is the one that is most effective at lowering your blood pressure without causing unwanted side effects. There are various specific reports about the benefits and potential harms of each of the specific classes of blood pressure medicines, but there is a huge volume of evidence supporting the fact that high blood pressure is deadly, and that lowering blood pressure saves lives. In the end, that is the true goal.
| High blood pressure guidelines | |
| Blood pressure | Classification |
| 140/90 or above | High |
| 120/80 to 139/89 | Prehypertension |
| 119/79 or below | Normal |
Calculate Your Risk for Heart Disease and Stroke with Hypertension

Comments 1
I am 40 years old, have congenital pulmonary artery branch stenosis in the right ventricle caused from a JAG1 gene mutation that runs deep in my family as discovered through genetic testing. In Dec. I took myself to the ER with a tightening chest pain/pressure between my breasts, shortness of breath, & an overall fatigue that I’ve never experienced before then. Prior to this day I had been getting really flushed in the face at nighttime for approximately 5 weeks, my BP has been fluctuating from 135/60 to 169/65, my left breast intermittently swells to twice it’s normal size ( I’m not in early menopause and it’s not cancer, I’ve been tested for both), & for the year previous to this incident my hair has been falling out so much that it’s what actually prompted me to start seeing my dr in the first place. Since that incident I still have a fatigue I’ve never had before, my hands are swollen from putting edema every morning upon waking, & my upon linking all my blood work from 2016 to now I have discovered my total cholesterol has been higher than 230 since 2018. I was a smoker for 23 years but have fully kicked the habit since this incident but I’m not on any cholesterol meds & never have been & my EKG from the ER visit came back with probable left atrial enlargement, RBBB, & LPFB. I haven’t been called by any doctors for an explanation of what that is/means and I just know I don’t feel the same since that incident & I’ve been experiencing a lot of forgetfulness & haven’t felt as sharp as usual but was told at the ER that my heart enzymes were good and it was just a viral infection. I think that my doctor is missing something. Should I be concerned or seeking a second opinion on this matter?