“Primary composite outcomes” (lumping complications together into one composite complication), allows shading of negative results that only become visible with careful study of a publication. In the CREST study described below, the authors combined procedural death, stroke and myocardial infarction together into a composite complication. In doing so they found no outcome difference between Carotid artery stenting (CAS) and Endarterectomy (CEA).
I strongly disagree with the conclusion as well as this kind of data manipulation, and will address the issue in my analysis of this paper:
Carotid Revascularization Endarterectomy vs. Stenting Trial (CREST)[1], a new study published in the latest issue of the NEJM, examined treatment outcomes for Carotid Artery Disease, a major cause of stroke. Stroke is the third most common cause of death among adults and the leading cause of long-term disability. CREST compared Carotid Artery Stenting (CAS) with Carotid Artery Stenting (CAS) as treatment of severe Carotid Artery Disease.
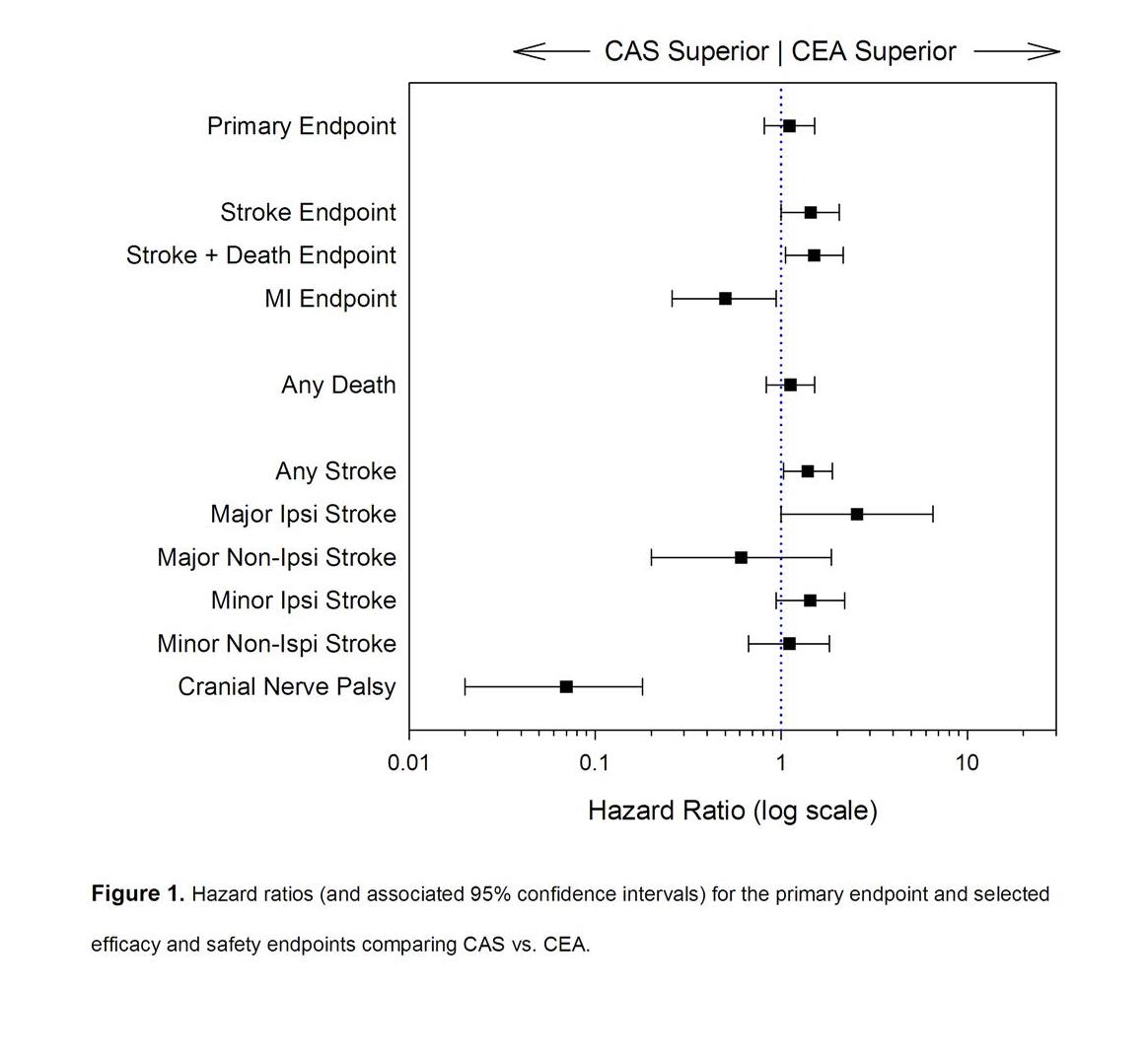
CAS was associated with more than double the mortality rate of CEA (Hazard Ratio (HR): 2.25) and an almost triple rate of ipsilateral stroke (HR: 2.67). The incidence of Myocardial Infarction (MI) in CSA patients occurred at half the rate of CEA treated patients.
| Carotid Artery Stenting (CAS) (N=1262) | Carotid Artery Endarterectomy (CEA) (N=1240) | Hazard Ratio (HR) CAS vs. CEA | P-Value | ||||
| Death | 9 | 4 | 2.25 | 0.18 | |||
| Complications | |||||||
| CVA | Any | Major Ipsilateral | Any | Major Ipsilateral | |||
| 52 | 29 | 1.79 | 0.01 | ||||
| 11 | 4 | 2.67 | 0.09 | ||||
| MI | 14 | 28 | 0.5 | 0.03 | |||
| Total Complications | 66 | 57 | 1.18 | 0.38 | |||
The results did not change substantially during the 4-yr follow-up period:
| Carotid Artery Stenting (CAS) (N=1262) | Carotid Artery Endarterectomy (CEA) (N=1240) | Hazard Ratio (HR) CAS vs. CEA | P-Value | ||||
| Death | 94 | 83 | 1.12 | 0.45 | |||
| Complications | |||||||
| CVA | Any | Major Ipsilateral | Any | Major Ipsilateral | |||
| 105 | 75 | 1.4 | 0.03 | ||||
| 16 | 6 | 2.56 | 0.05 | ||||
| MI | NA | NA | NA | NA | |||
| Total Complications | 105 | 75 | 1.11 | 0.51 | |||
However, despite this the authors concluded that “… CREST results indicate that carotid-artery stenting and carotid endarterectomy were associated with similar rates of the primary composite outcome — periprocedural stroke, myocardial infarction, or death and subsequent ipsilateral stroke — among men and women with either symptomatic or asymptomatic carotid stenosis. However, the incidence of periprocedural stroke was lower in the endarterectomy group than in the stenting group, whereas the incidence of periprocedural myocardial infarction was lower in the stenting group, … with younger patients having a slightly better outcome with carotid artery stenting and older patients having a better outcome with carotid endarterectomy…”
The study was supported by Abbott Vascular Solutions (formerly Guidant), including donations of Accunet and Acculink systems (the stents used), equivalent to approximately 15% of the total study costs.
An editorial[2] accompanying this article contradicted the CREST conclusions: … “the results are broadly consistent with those in previous trials. Namely, carotid-artery stenting is associated with a higher periprocedural risk of stroke or death, a difference that was still significant at 4 years. A recent meta-analysis of 11 randomized trials performed through 2009 (not including CREST) showed that carotid endarterectomy was superior to carotid-artery stenting, … We conclude that until more data are available, carotid endarterectomy remains the preferred treatment for most patients with symptomatic carotid stenosis”…
Remarks
I agree for the most part with the editorial but would the additional comments:
Treatment of Carotid disease has as goal the prevention of stroke through restoration of blood flow.
- Major Ipsilateral stroke often translates into a permanent disability such as hemiparesis. Prevention of this complication is the one and only goal of any carotid intervention.
- Peri-operative MI is a rare event, rarely of clinical consequence, and largely preventable in the hands of an experienced surgical and anesthesia team.
- The CREST analysis suggests that Death, Stroke and peri-procedural MI are equal complications, an absurd conclusion.
- Even though the more than double CSA mortality rate did not reach statistical significance in this study, it has in a number of other publications.
The Appendix listed together with the CREST publication shows the following[3]:
Somehow this page did not make it to the article. Why? Is it because the authors thought this to be meaningless information, or is it because the results are contradictory to the wished-for corporate sponsored outcomes?
As a surgeon with lots of “carotids” under my belt, one of my problems was to decide what to do first, CABG or CEA, since most of my patients had CAD as well as Carotid disease. Modern surgical techniques are so good that peri-operative stroke was not an issue: I cannot remember a single stroke in my patients (nor any mortality). As a procedure, it took about 45 minutes (“skin-to-skin”) to do the operation, discharging the patient 12-24 hours later. I doubt a stent placement can be done any quicker, and it certainly costs a lot more than two sutures and the occasional patch (the cost of OR and Lab estimated as equivocal).
So what do you prefer, an expensive stent with more than double the mortality and an almost triple stroke rate, in addition to which patients now need to be managed on a regimen of anti-platelet drugs with all the associated risks (thrombosis etc.)?
And what about another industry sponsored study only confirming what so many other investigations have found, i.e. that CEA is a superior treatment option for carotid artery disease? Or the authors’ conclusions, contradicting their own results?
DR T
[1] Stenting versus Endarterectomy for Treatment of Carotid-Artery Stenosis, Thomas G. Brott, M.D.et al, (N Engl J Med 363:11-23)
[2] Carotid-Artery Stenting in Stroke Prevention, Stephen M. Davis, M.D., and Geoffrey A. Donnan, M.D., (N Engl J Med 36: 80-82)
[3] Stenting versus Endarterectomy for Treatment of Carotid-Artery Stenosis. N Engl J Med 2010;363:11-23 Supplementary Appendix, Brott TG et al. (N Engl J Med 363:11-23)

