Palpitations are feelings that your heart is skipping a beat, fluttering, or beating too hard or too fast. You may have these feelings in your chest, throat, or neck. They can occur during activity or even when you’re sitting still or lying down:
Many things can trigger palpitations, including:
- Strong emotions
- Vigorous physical activity
- Medicines such as diet pills and decongestants
- Caffeine, alcohol, nicotine, and illegal drugs
- Certain medical conditions, such as thyroid disease or anemia (a low blood count).
These factors may make the heart beat faster or stronger than usual, or they cause occasional extra heartbeats. In these situations, the heart is still working normally, and the palpitations usually are harmless.
Sometimes palpitations are symptoms of an arrhythmia. An arrhythmia is a problem with the rate or rhythm of the heartbeat.
Some arrhythmias are signs of heart conditions, such as heart attack, heart failure, heart valve problems, or heart muscle problems. However, less than half of the people who have palpitations have arrhythmias.
People can reduce or prevent palpitations by avoiding things that trigger them (such as stress and stimulants) and treating related medical conditions.
Outlook
Palpitations are very common. They usually aren’t serious or harmful, but they can be bothersome. If you have them, your doctor can determine whether you need treatment or ongoing care.
How Are Palpitations Diagnosed?
Your doctor will first want to find out whether your palpitations are harmless or related to a more serious heart problem. To do this, he or she will ask about your symptoms and medical history, do a physical exam, and recommend several basic tests.
This information may point to a heart problem as the cause of your palpitations. If so, your doctor may recommend more tests. These will help show what the problem is and how to treat it.
The cause of palpitations may be hard to diagnose, especially if symptoms don’t occur regularly.
Specialists Involved
Several types of doctors may work with you to diagnose and treat your palpitations. These include a:
- Primary care doctor
- Cardiologist (a doctor who specializes in diagnosing and treating heart diseases and conditions)
- Electrophysiologist (a cardiologist who specializes in the heart’s electrical system)
Medical History
Your doctor will ask questions about your palpitations, such as:
- When did they begin?
- How long do they last?
- How often do they occur?
- Do they start and stop suddenly?
- Does your heartbeat feel steady or irregular during the palpitations?
- What other symptoms do you have when you get palpitations
- Do your palpitations have a pattern? For example, do they occur when you exercise or drink coffee? Do they happen at a certain time of day?
Your doctor also will ask you about your use of caffeine, alcohol, supplements, and illegal drugs.
Physical Exam
Your doctor will take your pulse to find out how fast your heart is beating and whether it’s beating with a normal rhythm. He or she also will use a stethoscope to listen to your heartbeat.
Your doctor may look for signs of other conditions (such as an overactive thyroid) that can cause palpitations.
Often, the first test that’s done is an EKG. This simple test records your heart’s electrical activity.
An EKG is used to detect and locate the source of heart problems. It shows how fast your heart is beating and whether its rhythm is steady or irregular. It records the strength and timing of electrical signals as they pass through each part of your heart.
Even if your EKG results are normal, you may still have a medical condition that’s causing palpitations. If your doctor suspects this is the case, you may have blood tests to gather more information about your heart’s structure, function, and electrical system.
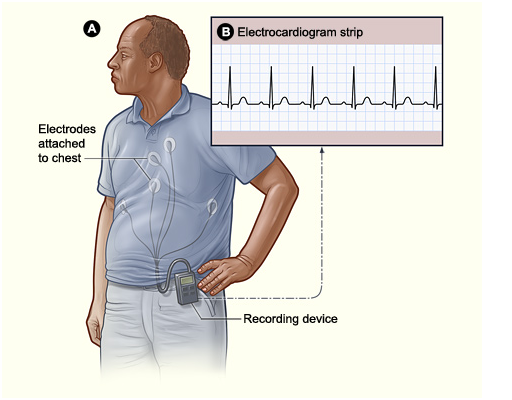
A Holter monitor is a small device that records your heart rhythm. You usually wear a Holter monitor for one to three days, and during that time, the device will record all of your heartbeats. A Holter monitor test is usually performed after a traditional test to check your heart rhythm (EKG) isn’t able to give your doctor enough information about your heart’s condition.
A Holter monitor has electrodes that are attached to your chest with adhesive and connected to a recording device. Your doctor uses information captured on the Holter monitor’s recording device to figure out if you have a heart rhythm problem.
While wearing a Holter monitor may be a little inconvenient, it’s an important test that may help your doctor diagnose your condition.
Reasons why a Holter monitor test is done include:
- Observe for cardiac irregularities, such as fast or slow heartbeat, extra beats or palpitations
- Evaluate effectiveness of cardiac medications
- Evaluate pacemaker functioning
- Determine if unexplained episodes of dizziness are related to heart problems
Once your monitoring period is over, you’ll go back to your doctor’s office to return the Holter monitor.
You’ll also turn in the diary you kept while you wore the Holter monitor. When the Holter monitor is interpreted, your doctor will compare the data from the recorder and the activities and symptoms you wrote down. If your heart rhythm changed while you completed strenuous activities or experienced symptoms, knowing that information can help your doctor diagnose your condition.
After your doctor has looked at the results of the Holter monitor recorder and what you’ve written in your activity diary, he or she will talk to you about your results. The information from the Holter monitor may reveal that you have a heart condition, or your doctor may need more tests to find out what may be causing your symptoms.
In some cases, your doctor may not be able to diagnose your condition based on the results of the Holter monitor test, especially if you didn’t have any irregular heart rhythms while you wore the monitor. Your doctor may then recommend an event recorder. You wear an event monitor as much as possible throughout the day, and push a button on a recording device you wear on your belt to record your heartbeat when you experience symptoms.
Holter Monitor
Figure A shows how a Holter monitor attaches to a patient. In this example, the monitor is clipped to the patient’s belt and electrodes are attached to his chest. Figure B shows an electrocardiogram strip, which maps the data from the Holter or event monitor.
Who Needs a Holter or Event Monitor?
Your doctor may recommend a Holter or event monitor if he or she suspects you have an arrhythmia. An arrhythmia is a problem with the rate or rhythm of the heartbeat.
Holter and event monitors most often are used to detect arrhythmias in people who have:
- Fainted or sometimes feel dizzy. A monitor may be used if causes other than a heart rhythm problem have been ruled out.
- Palpitations that recur with no known cause. Palpitations are feelings that your heart is skipping a beat, fluttering, or beating too hard or fast. You may have these feelings in your chest, throat, or neck.
People who are being treated for heart rhythm problems also may need to use Holter or event monitors. The monitors can show how treatments are working.
Heart rhythm problems may only occur at certain times, such as during sleep or physical exertion. Holter and event monitors record your heart rhythm while you do your normal daily routine. This allows your doctor to see how your heart responds to different daily activities, which can help diagnose the problem.
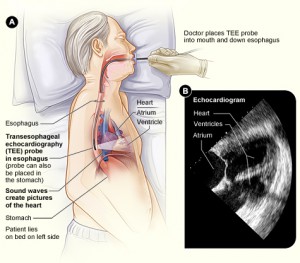
Echocardiogram (Echo; TransThoracic Echocardiogram; TTE)
An echocardiogram is a specialized ultrasound machine that creates a video image of the beating heart. This non-invasive test is often used to identify problems with heart muscle and valves.It is a fast, easy and painless evaluation that uses ultrasound waves to produce images of the heart, evaluate your heart’s performance as well as the inside, including the heart chambers and valves. An echo may sometimes also be used to look for the cause of a heart murmur, to check the size of the heart chambers, for fluid around the heart, or to inspect the pumping capability of the heart if a patient is short of breath or has other symptoms, f.i. during exertion.
Another type of echocardiogram is a transesophageal echocardiogram also referred as a TEE. This test may be recommended to evaluate different structures in the heart such a valves or blood clots. The esophagus sits behind the heart and by advancing the echo transducer down the esophagus common obstructions are avoided such as the lungs and ribs. This provides clearer images.



Comments 15
Pingback: Mitral Valve Prolapse (MVP) | Cardiac Health
Hello I’m 30 years old and about 4 months ago I went to the dentist to have 3 bad teeth cut out the dentist wouldn’t do the surgery because my heart was going erratic so I went to my family doctor and they did EKG and it come back saying I had sinus tachycardia paired with pvcs so they did an echo everything come back normal I’m just having ALOT of pvcs so they gave me a holter monitor it came back showed the same thing a lot of pvcs so then I had a cardiac MRI came back that everything was normal just a lot of pvcs now my doctor wants to do an ablation procedure to correct the pvcs but I have chronic constipation and I know the medicine I’m taking is causing the constipation but can my 3 bad teeth be causing this heart arrhythmia problems or the chronic constipation? I’m worried if I go through with this procedure to correct the heart problems that it will cause irreversible heart damage and that my teeth or chronic constipation was the cause of the heart problems to begin with?? Please help I don’t know what to do
Have you ever been test or worked up for either dysautonomia or POTS (postural orthostatic tachycardia syndrome)? It might be worth exploring and then asking your doctor about.
I have had 2atteps at having a 24heart monitor fitted both attemps would not work so the machine was not fitted!has anyone else had this experience and what happened next?a echocardiogram appears reasonAbly good for my age of 88.5 so why will happen next?
about a year ago i started havining these weird sensations in my upperleft chest. to me they feel like flutters/ bubbles popping in my chest. have done 2 EKG, blood work and xray and they found everything to be normal. did not feel them for a few months now all of a sudden they are back. i have no other symptoms. any ideas why this is happening. i mean 90% of the times i am relaxed when this occur. please help i am worried.
i am only twenty years old physically fit dont know y this is happening again
I have been having the same thing. It feels like bubbles popping. Did you ever find out what it was?
I have a similar question as Isopura. Why would I need to have an echocardiogram AND a holter monitor? The copays alone are over $500. I’ve already been diagnosed with A-Fib following an EKG. Do I really need all these tests?
Ive had ECGs, 24hr, 5 day holters, EKGs n they found three small leaky valves- also its an alleged electric fault making my heart weird but im supposed to luve eith these demons? Why won’t they fix the valves? No help. Ive been bedridden 4 years, list 5 st and cant walk anymore due to terror n how bad the palps have got now. Taken over my existence. Pills dont work and my heart sometimes drops teally sliw ( no dizzy soells but one beat to every 4 secs is terrifying).
I have begged n pleaded, offered to pay to stay inhospitable just for a frw days to feel safe but they say no. I cannot take anymore/ is this it? At 46 how my life goes on till death? Lying in a filthy bed too scared to move? I used to do karate, ride, run… one day i had what thry thought was sn afib attack from nowhere. Sincd then the palps never stopped. Im dying.. dying as ive given up in ever luving again.
Hi, I am 42 yr old woman and I am going through similar situation where palpitations have started a few months back and now don’t stop. It is a terrible feeling, I keep going because of my kids. Don’t give up, the way I look at it is, nothing has happened to me yet and if it does than I will figure it out. I also have a thyroid issue that sometimes goes off and puts everything out of whack like these symptoms in my heart. It has just gone off again 3 months ago so could be my cause, waiting to see if my change in meds will help. If you have not ever had your thyroid checked I would recommend it. Checked through blood work, ask your doc to do a TSH test along with a T3, T4 test. The thyroid can cause a lot of issues as it controls 80 functioning parts of your body, you cannot live with out it. Good luck. Don’t give up on life by living in fear. Worst case scenario you start doing things an heaven forbid something goes wrong and your require emergency attention, that will get you admitted to the hospital, that way they might run further tests for your peace of mind. All the best. J
I’m a 30 yo female with a bmi of 32. I was taking the diet pill phenteramine (addipex) for approximately 3 months (prescribed by my primary doctor) when I started to experience palpitations (skipped heart beats) during and immediately following intense cardio workouts (heart rate ave 150bpm) 3x a week. I stopped taking the drug and my primary care doctor prescribed a 24hr holter monitor. I didn’t receive the specific results of the test but I was informed that my hr exceeded 160bpm (during my cardio workout) and that the “irregularities” were less than 1%. My primary care doctor then recommended that I see a cardiologist. The cardiologist reviewed my holter monitor results (with less than 1% irregularities) and wrote me a prescription to receive an echocardiogram. The eco will cost me over $200 and I rather not spent the money unnecessarily. Would you suggest that I receive the eco? I have had palpitations one time since I stopped taking phentermine (during a workout) and I have not had palpitations in over 6 months. I have only ever experienced palpitations during intense cardiac activity. Also do you think that the doctors are using the correct standards and prescriptions for diagnosing a pt with palpitations? Would you do anything differently.
What if I’ve done all these test and everything comes back negative .
Author
As you can read, these tests are to confirm or exclude something serious is wrong with your heart. the frequency of bothersome palpitations can be reduced with some medications (as discussed in this post), but whether all necessary tests have been done only your doctor knows.
Hope this helps,
Dr T
Indecently had a hear scare and visited the hospital. I did an ECG bio Chen test an xray and a cardiac enzyme test which all came negative. What I experienced were palpitations, tightness in my left breast area including my shoulder left arm and neck and heart burns also pain in my back. Before then I checked my bp n was OK. But after this experience my bp at the hospital was 140-90. I have bn discharged n am back home but I still do have the palpitations, heart burns and the pain just that the pains are more mild. Am on diclo, pmol, amoxyclin, amlodipine, creator,n medications for GERD. I still don’t feel n fine n I do feel bits of dizziness
Author
It also appears your treatment is not finished. You need to go back to your provider for additional support.
Dr T