There is more and more evidence of the superiority of medical therapy over stenting, not only with coronary artery disease, but also with stenotic arteries in your brain: The 30-day rate of stroke or death associated with stenting (14.7%) is nearly 2.5 times as high as the 6% rate associated with stenting in high-risk patients with a 70 – 90 % severe intracranial arterial stenosis.
These types of patients are at a high risk of a second stroke (approximately 23% at 1 year), despite treatment with aspirin and standard management of vascular risk factors. Two strategies have been used to treat these high-risk patients: Stenting, and medical management that combines platelet therapy with management of risk factors.
In the Sept. 7 New England Journal of Medicine issue, the Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) compared stenting plus aggressive medical management with aggressive medical management alone in high-risk patients.
SAMMPRIS compared the treatment of 451 such patients with a recent transient ischemic attack (TIA) or stroke, but on April 5, 2011, the trial’s monitoring board recommended that enrollment be stopped because of safety concerns regarding the risk of peri-procedural stroke or death in the stent group:
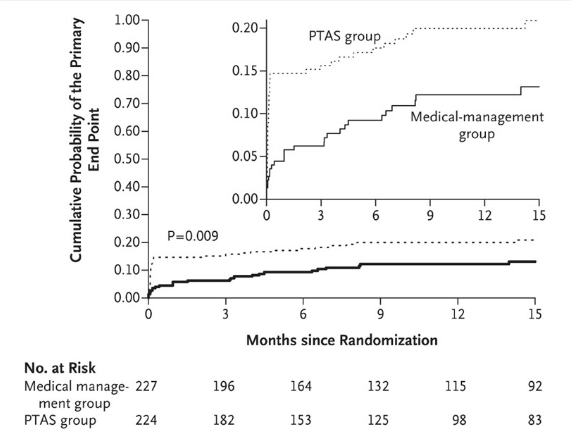
Kaplan–Meier Curves for the Cumulative Probability of the Primary End Point, According to Treatment Assignment.
Improving blood flow has not shown to be a benefit in other trials such as the Carotid Occlusion Surgery Study (COSS). Although the bypass surgery in COSS improved perfusion of blood to the brain, it was ineffective, as compared with medical therapy, in preventing other strokes.
References:
