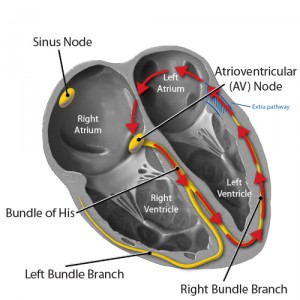
Patients with Wolff-Parkinson-White (WPW) syndrome have an extra connection in their heart, called an accessory pathway, that allows electrical signals to bypass the Atrio-Ventricular node and move from the atria to the ventricles faster than usual. The accessory pathway (called Bundle of Kent) may also transmit electrical impulses abnormally from the ventricles back to the atria. This extra connection can disrupt the coordinated movement of electrical signals through the heart, leading to an abnormally fast heartbeat (tachycardia) and other arrhythmias.
Resulting symptoms include dizziness, a sensation of fluttering or pounding in the chest (palpitations), shortness of breath, and fainting (syncope).The most common arrhythmia associated with Wolff-Parkinson-White syndrome is called Paroxysmal Supraventricular Tachycardia (PSVT).
Below is an animation from The National Heart, Lung & Blood Istitute of WPW:
Some patients with WPW are at high risk for Sudden Cardiac Death (SCD). Risk factors to look for include previous episodes of unexplained syncope (fainting) or palpitations, and what the EKG looks like during PAT:
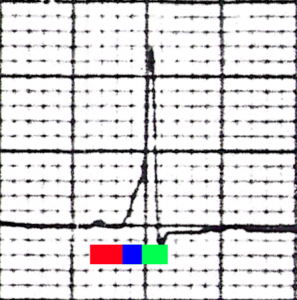
Characteristic EKG finding in WPW Syndrome. The red bar represents the PR interval of 0.1 seconds (100 milliseconds). The blue bar represents the slurred upstroke in the QRS complex that is found in WPW syndrome, known as the delta wave. The combination of the blue bar and the green bar make up the QRS complex, which is prolonged (160 milliseconds).
Patients with WPW need evaluation that includes an “EP study”, and occasionally a procedure called “radio frequency ablation“.


Comments 1
The labelling of the branches is incorrect. Conducting system of LV labelled as RBB and vice versa.