SYNTAX was an 1800-patient trial randomizing patients with left main coronary disease and/or three-vessel disease to either CABG or PCI using the Taxus drug-eluting stent (DES).
Findings
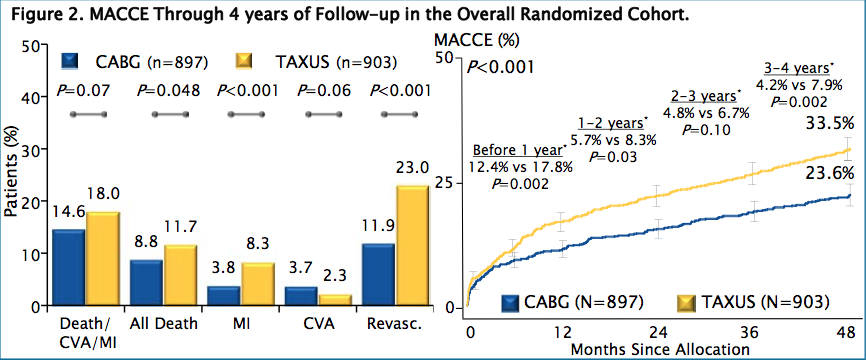
In patients with severe, multi-vessel coronary disease, coronary artery bypass grafting (CABG) continues as the standard of care of revascularization. Death and MI rates did become significantly greater in the PCI group after four years:
| Outcome | CABG surgery, n=819 (%) | PCI, n=879 (%) | p |
| MACCE | 23.6 | 33.5 | <0.001 |
| Death/stroke/MI | 14.6 | 18 | 0.07 |
| All-cause mortality | 8.8 | 11.7 | 0.048 |
| Cardiac death | 4.3 | 7.6 | 0.004 |
| Stroke | 3.7 | 2.3 | 0.06 |
| MI | 3.8 | 8.3 | <0.001 |
| Repeat revascularization | 11.9 | 23 | <0.001 |
Three Vessel Disease
The 3VD subgroup patients by SYNTAX Score showed similar MACCE in patients with low scores (0-22: CABG 24.7% vs. PCI 30.4%, p=0.27); whereas both MACCE and mortality were increased in PCI patients with intermediate scores (23-32: 17.9% vs. 33.3%, p<0.001 and 6.8% vs. 12.7%, p=0.048), and with scores ≥33 (21.2% vs. 37.9%, p<0.001 and 6.5% vs. 14.5%, p=0.02):
|
Adverse Event Rates at 4 years in the 3VD cohort |
|||||
| CABG (n=549) | PCI (n=546) | CABG (n=549) | PCI (n=546) | ||
| MACCE | 21.00% | 33.7%* | Stroke | 3.40% | 2.80% |
| Death/Stroke/MI | 12.60% | 18.6%* | MI | 3.30% | 9.0%* |
| Death | 7.30% | 11.9%* | Repeat Revascularization | 10.20% | 22.8%* |
|
MACCE: Major adverse cardiac and cerebrovascular events including all-cause death, stroke, myocardial infarction, repeat revascularization. Time-to-event rates at 4 years (*: P<0.05 from log-rank or chi-square test.) |
|||||
Left Main Disease
Four-year MACCE and the composite of death/stroke/MI were similar in ULMCA- PCI and CABG-treated patients (Table). Stroke was significantly increased in the CABG group and repeat revascularization was increased in the PCI arm at 4 years. MACCE was similar between groups in patients with low or intermediate SYNTAX Scores (0-32: 29.0% vs. 27.6%, p0.65) but significantly increased in PCI patients with high scores (≥33: 26.3% vs. 42.6%, p=0.003).
|
Adverse Event Rates at 4 years in the LM cohort |
|||||
|
CABG (n=348) |
PCI (n=357) |
CABG (n=348) |
PCI (n=357) |
||
|
MACCE |
27.80% |
33.2% |
Stroke |
4.30% |
1.50%* |
|
Death/Stroke/MI |
17.70% |
17.1% |
MI |
4.80% |
7.2% |
|
Death |
11.20% |
11.4% |
Repeat Revascularization |
14.60% |
23.5%* |
| MACCE: Major adverse cardiac and cerebrovascular events including all-cause death, stroke, myocardial infarction, repeat revascularization.
Time-to-event rates at 4 years (*: P<0.05 from log-rank or chi-square test.) |
|||||
Comments
Differences between the two groups:
- Stroke rates were now no longer significant
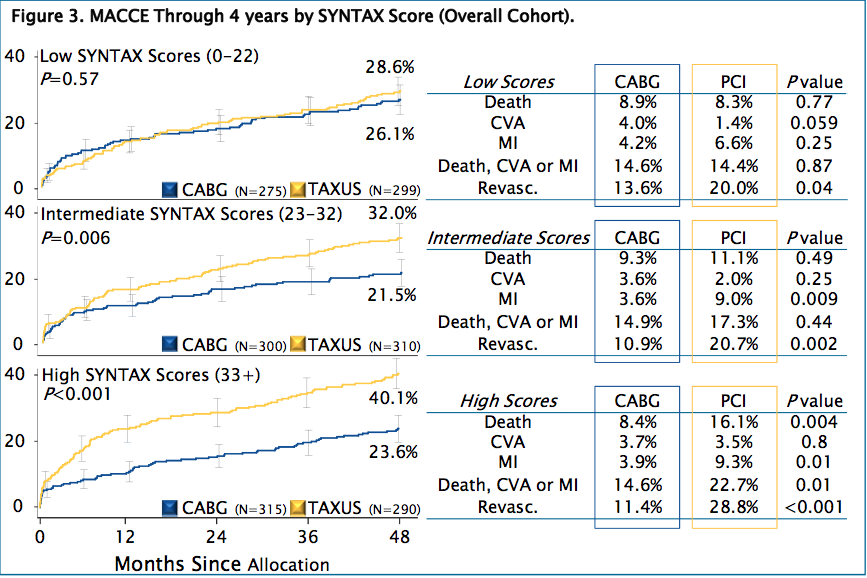
- Intermediate SYNTAX score (23 – 32): a highly significant difference in MACCE rate (CABG 21.5% vs. PCI 32%; p=0.006).
- High SYNTAX score (>33), mortality was doubled in the PCI group compared with CABG (16.1% vs. 8.4%; p=0.04) and MI was two to three times higher with PCI than with CABG (9.3% vs. 3.9%; p=0.01).
- In this highest-risk group, even the end point of death/stroke/MI became significantly higher with PCI, (22.7% vs. 14.6%; p=0.01), and MACCE were much higher (40.1% vs. 23.6%; p<0.001), driven in large part by a 17% higher rate of revascularization
Conclusions
Four-year results suggest that CABG remains the standard of care for patients with complex lesions (intermediate or high SYNTAX Score). With less complex disease (low SYNTAX Scores), PCI is an acceptable revascularization alternative.

Comments 2
Pingback: The MASS II Study - Cardiac Health
Pingback: Optimal Medical Therapy with or without PCI for Stable Coronary Disease - Cardiac Health