Heart Attack (Myocardial Infarct)
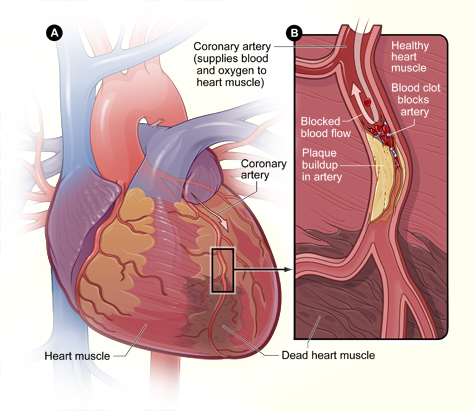
Acute myocardial infarction (AMI), commonly known as a heart attack, is the interruption of blood supply to part of the heart, causing some heart muscle cells to die. It is most commonly due to occlusion (blockage) of a coronary artery following the rupture of a vulnerable atherosclerotic plaque, which is an unstable collection of lipids (fatty acids) and white blood cells (especially macrophages) in the wall of an artery. The resulting ischemia (restriction in blood supply) and oxygen shortage, if left untreated for a sufficient period of time, can cause damage or death (infarction) of heart muscle tissue (myocardium).
(From: From Wikipedia, the free encyclopedia)
The most common symptom of a heart attack in both men and women is some type of pain, pressure or discomfort in the chest. But it’s not always severe or even the most prominent symptom, particularly in women. Women are more likely than men to have signs and symptoms unrelated to chest pain, such as:
- Neck, shoulder, upper back or abdominal discomfort
- Shortness of breath
- Nausea or vomiting
- Sweating
- Lightheadedness or dizziness
- Unusual fatigue
These signs and symptoms are more subtle than the obvious crushing chest pain often associated with heart attacks. This may be because women tend to have blockages not only in their main arteries, but also in the smaller arteries that supply blood to the heart — a condition called small vessel heart disease.
Many women tend to show up in emergency rooms after much heart damage has already occurred, because their symptoms are not those typically associated with a heart attack.
Heart disease risk factors for women
Although the traditional risk factors for coronary artery disease — such as high cholesterol, high blood pressure and obesity — affect women and men, other factors may play a bigger role in the development of heart disease in women. For example:
- Metabolic syndrome — a combination of fat around your abdomen, high blood pressure, high blood sugar and high triglycerides — has a greater impact on women than on men.
- Mental stress and depression affect women’s hearts more than men’s.
- Smoking is a greater risk factor for heart disease in women than in men.
- Low levels of estrogen after menopause pose a significant risk factor for developing cardiovascular disease in the smaller blood vessels (small vessel heart disease).
A diagnosis of myocardial infarction can be made after evaluation of a patient’s complaints, an examination and a variety of tests:
- Clinical history of angina lasting for more than 20 minutes
- Changes in serial EKGs:
Diagnosis
Medical societies recommend that the physician confirm that a patient is at high risk for myocardial infarction before conducting imaging tests to make a diagnosis.[66][67][68][69] Patients who have a normal ECG and who are able to exercise, for example, do not merit routine imaging.[66][67] Imaging tests such as stress radionuclide myocardial perfusion imaging or stress echocardiography can confirm a diagnosis when a patient’s history, physical exam, ECG and cardiac biomarkers suggest the likelihood of a problem.[66][67]
The diagnosis of myocardial infarction can be made after assessing patient’s complaints and physical status. ECG changes, coronary angiogram and levels of cardiac markers help to confirm the diagnosis. ECG gives valuable clues to identify the site of myocardial damage while coronary angiogram allows visualization of narrowing or obstructions in the heart vessels.[70] At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.
A chest radiograph and routine blood tests may indicate complications or precipitating causes and are often performed upon arrival to an emergency department. New regional wall motion abnormalities on an echocardiogram are also suggestive of a myocardial infarction. Echo may be performed in equivocal cases by the on-call cardiologist.[71] In stable patients whose symptoms have resolved by the time of evaluation, Technetium (99mTc) sestamibi (i.e. a “MIBI scan”) or thallium-201 chloride can be used in nuclear medicine to visualize areas of reduced blood flow in conjunction with physiologic or pharmacologic stress.[71][72] Thallium may also be used to determine viability of tissue, distinguishing whether non-functional myocardium is actually dead or merely in a state of hibernation or of being stunned.[73]
WHO criteria[74] formulated in 1979 have classically been used to diagnose MI; a patient is diagnosed with myocardial infarction if two (probable) or three (definite) of the following criteria are satisfied:
- Clinical history of ischaemic type chest pain lasting for more than 20 minutes
- Changes in serial ECG tracings
- Rise and fall of serum cardiac biomarkers such as creatine kinase-MB fraction and troponin
The WHO criteria were refined in 2000 to give more prominence to cardiac biomarkers.[75] According to the new guidelines, a cardiac troponin rise accompanied by either typical symptoms, pathological Q waves, ST elevation or depression, or coronary intervention is diagnostic of MI.
Read more: http://www.answers.com/topic/myocardial-infarction#ixzz2DYD7pKvB
EKG changes after a heart attack (from Myocardial Infarction)

With an infarction changes in the QRS-complex are seen. The dead muscle tissue is no longer “electrically active”. The EKG lead above the necrotic tissue looks through a window of dead muscle tissue right into the heart cavity, causing a negative Q-wave.
While the vast majority of abnormal Q waves are due to myocardial infarction (MI), others can be caused by other cardiac illnesses such as hypertrophic cardiomyopathy (the result of long-standing high blood pressure) and may simulate anterior or inferior myocardial infarction.
An unexpected change such as this on a routine EKG should be evaluauted with a cardiology consultation, a stress ECHO, and probably a CTCA Scan.
- Rise and fall of serum cardiac blood tests such as CPK and troponin levels.
Other tests are sometimes performed to check heart and cardiac valve function as well as the coronary artery anatomy and location of blockages:
Treatment aims to salvage as much heart muscle as quickly as possible (“time is muscle”), preserve heart function and to prevent complications such as heart failure. Oxygen, aspirin, and nitroglycerin (NTG) are used routinely as an initial therapy, often first given in the ambulance.
Acute Coronary Artery Syndrome (ACS) is a medical emergency and requires immediate hospital admission:
STEMI
If the EKG confirms changes suggestive of a heart attack, medication is injected that dissolves blood clots obstructing the coronary arteries, or a Percutaneous coronary intervention (PCI) may be performed in STEMI, but to be effective requires to be performed in a very limited time span.
NSTEMI and NSTE-ACS
If the ECG does not show typical changes, the term “non-ST segment elevation ACS” is applied. The patient may still have suffered a “non-ST elevation MI” (NSTEMI). The accepted management of unstable angina and acute coronary syndrome is treatment with medications alone.




Comments 1
Pingback: Chronic anticoagulation in atrial fibrillation - Cardiac Health